Postpartum Care
After the Baby Comes: Optimizing Postpartum Care
The process of pregnancy and childbirth consumes an enormous amount of mental energy, physical resources, and vital nutrients even in the most ideal circumstances. In the modern high-stress environment, this phase of life is inevitably physically and emotionally exhausting. Many cultures that value women have healing supportive traditions during the postpartum time. Chinese Medicine has a comprehensive philosophy devoted to the process of replenishing and restoring resources for the mother, and by association, the new child. You may have heard the phrase Zuo Yue Zi which literally translates to “sitting through the lunar cycle”, referring to the crucial month post-partum to rest and replenish. During this time, a new mother’s sole job should be to rest, heal and be with her baby. Special foods, herbs, gentle exercises, and acupuncture or moxibustion treatments (a type of warming therapy) are given to nourish both mother and child.
Resting after giving birth is important to avoid muscle strain and allow the organs to return to pre-pregnancy positions. Traditional recovery strategies include abdominal wrapping and strict bed rest. Some new parents benefit from exercises such as yoga or Pilates; we have a referral network with wonderful local instructors who can safely guide these exercises without causing injury. At MHS, new parents are always treated as unique individuals and we make recommendations based on every person’s own postpartum needs.
According to the traditional Chinese view, acupuncture and herbal medicine are an essential part of postpartum care. There are a number of herbal formulas to help replenish physical resources after having a baby. One of the most common formulas is Ba Zhen Tang, or 8 Treasures Decoction. Our practitioners frequently make custom herbal formulas to meet the very personalized needs of each patient. And as always, all herbs dispensed by our office are from high-quality sources that test for pesticides, preservatives, and heavy metals. We also recommend a diet rich in blood-building foods such as grass-fed meat, bone broth, cooked green veggies, beets, collagen, healthy fats, nuts and seeds, and fermented foods. Again, though all healthy diets have things in common, we make recommendations based on each person’s specific health needs.
Chinese medicine can also support various problems that may arise after giving birth. The most common issues we see include post-partum depression, trouble with breastfeeding, lactation pain, low energy, body pain, digestive issues, and the various problems associated with lack of sleep. Traditional Chinese Medicine has been effectively dealing with these symptoms for thousands of years, with a combination of herbal formulas, acupuncture, moxibustion, diet therapy, and helping to configure each individual’s proper support system. No two pregnancies are the same (even within the same person), and every new parent’s needs are unique. There is no one size fits all approach to postpartum care, and our practitioners are here to support you through this crazy, exhilarating, wonderful time.

Children’s Health
Many parents seek alternatives to conventional treatments to help their children with a variety of pediatric illnesses. Asthma, allergies, skin conditions, ADHD, digestive disorders and anxiety may be symptomatically treated with medications, but the potential for lifetime dependence on drugs leads families to look for a more natural solution that hopefully also addresses the underlying root of the disorder. Chinese medicine can be a valuable tool in a parent's toolbox to naturally support the health and well-being of their children.
Can my child REALLY get acupuncture? Yes. Infants, children and teens receive acupuncture in different ways depending on their needs. Any child can get acupuncture, with needles being inserted and quickly removed, or retained for a short duration, depending on the child's comfort and ability to be still. Both ways are effective, and one method is not superior to the other when it comes to treating children.
What other things can we use instead of or alongside acupuncture? Chinese herbal medicine, homeopathy, and nutritional supplements are all important additional tools for treating children. Herbs, supplements, and homeopathy provide daily support for a child's condition when they're not in the treatment room. These come as teas, pills or dissolvable pellets, so there are different options depending on your child's age and comfort. Compliance with their herbal formula will be important to the success of their treatment; while Chinese herbs can be bitter, your practitioner will help your child find easy and creative ways to take them!
I have a feeling I need to change my child's diet; can you help with that? Nutritional counseling is a big part of all treatments at MHS no matter the age of the patient. Most pediatric treatment strategies succeed because of the willingness of a child (and their family) to work with food as the easiest and most available form of medicine! Your practitioner will help coach you on the best diet for your child's condition.
When you're bringing your child in for acupuncture, here's what you need to know BEFORE their appointment:
If you're bringing your child in for acupuncture for the first time it is important that you have a conversation with them about what will happen BEFORE they come for their treatment. We recommend that you prepare your child for the fact that there will be needles. Explain that the needles are the size of a cat whisker, that the needles will go in just under their skin and come right out, and that they are painless. Your wording is important here. If you feel your child will react better to a word other than “needle” then use whatever language will help them feel comfortable (e.g. pin, Chinese medicine tool, rainbow unicorn energy wand… you know your child better than we do). Kids often ask whether it will hurt, and the answer is no! They will feel a “tap” when the needle is inserted but beyond that, they won't feel much of anything at all.
It's not uncommon for children to be immediately averse to the idea of getting acupuncture, therefore many parents find that offering some kind of small reward on the condition of completing their first treatment (a treasured snack… that coveted toy or game…) provides enough incentive for the child to be brave and go for it. Some children find comfort in holding on to a stuffed animal or blankie during the session.
Before their visit, watch these videos with your child so they know what the needles look like and see how easy it is:
https://www.youtube.com/shorts/IuXMBN8SL1Y
https://www.youtube.com/watch?v=O3IawxibRzs
Please remember that an appointment's time is finite; if a fair amount of time is spent on parents and practitioner trying to convince the child to get acupuncture, in the end there may not be enough time for the actual treatment. Talking to kids about acupuncture empowers them to be prepared for their visit and gets their bodies, minds and energy ready for what will happen. Children who are prepared for acupuncture can be more consistent with treatment, are less afraid at their first visit (and are genuinely excited to try it) and therefore have better outcomes.

Emotional Health
Depression, anxiety and stress affect people of every age, race and social status. NIH data from 2017 showed that over 7% of all U.S. adults suffered at least one major depressive episode, and over 19% had anxiety disorders in the last year. Because Traditional East Asian Medicine seeks to address the individual as a whole, it has many methods for treating problems of emotional health. Rather than isolating symptoms as “physical,” “mental,” or “emotional,” we look at the whole person, making the connection between all body systems. Whether a patient has suffered from anxiety their whole life, is in the middle of a stressful event at home or work, is having an acute battle with post-partum depression, or any other situation where their emotional stability is being challenged, Traditional East Asian Medicine may provide immediate and lasting relief.
How does Western Medicine Treat Mental-Emotional Conditions?
Typically, conventional medicine recommends cognitive therapy, medications, or a combination thereof, if warranted. Therapy can be provided by psychologists, licensed professional counselors, licensed clinical social workers, or even by psychiatrists. Psychiatry generally emphasizes the use of medications to treat mental-emotional conditions, and there are a wide range of them that can prescribed. SSRI’s are one category of medications that affect the use of serotonin (the neurotransmitter often associated with happiness), but there are other categories of drugs like SSNRI’s, MAOI’s, Tricyclics, and benzodiazepines, used for different kinds of depression, anxiety, bipolar disorders, and even pain syndromes. Medications can be extremely helpful, especially when a patient feels they cannot function in life because of their symptoms. However, the medications can come with a list of side-effects—among them weight gain, loss of libido, and a feeling of “flatness”—that many patients find are not a good trade-off for any well-being they provide. The other downfall to medications is that they can be difficult to discontinue even if the patient is ready for that step. In fact, many patients end up staying on medications not because they still feel the need, but because when they try to get off them, their symptoms get worse, and the withdrawal is difficult or even painful.
Traditional East Asian Medicine’s View of the Emotions
According to Chinese medical theory, when emotions are out of balance, they are deemed to be a cause of disease, not unlike how a virus or bacteria causes disease. Emotions can come from outside us, as in the case of traumatic events or stressful situations, or they can be internally generated and perpetuated such as worry or fear that is disproportionate to the cause. Either way, unbalanced emotions affect the body in various ways, and it is the goal of the Traditional East Asian Medicine practitioner to help restore them to a more harmonious state.
Traditional East Asian Medicine Treatment Strategies
Acupuncture is an important part of restoring emotional balance. It modulates the body’s stress response, balances the sympathetic and parasympathetic nervous systems, supports healthy adrenal function, and calms the spirit. The acupuncture treatment itself is extremely relaxing, and it helps give the body a calm place to “resource” in times of stress or anxiety. Currently, acupuncture is being used across the world to help soldiers with PTSD. Chinese herbal medicine and nutritional supplements are safe and effective tools to use on a daily basis for addressing the roots of anxiety, depression and stress. There are many products on the market that tout the ability to reduce symptoms, but a good Chinese Medicine practitioner will always tailor herbal formulas to an individual’s specific case, which makes for more successful and lasting results. Nutrition is critical when treating disorders of emotional health. The right foods can make a tremendous difference in how stressed or anxious one feels and can support a more balanced and stable mood. Simple dietary changes can make a big difference in the reduction of symptoms like panic, lethargy, irritability and instability. Using Western and Eastern Medicine: Sometimes, patients are using antidepressants or anti-anxiety medication, yet continue to experience symptoms. Traditional East Asian Medicine can be the missing link to help treat the root of the problem while the medication tones down the symptoms. We work with many patients who, with the help of their prescribing physicians, relied on Traditional East Asian Medicine to wean off antidepressants, or as a form of support while they went through the uncertain process of finding the right medication or dosage. Others use Traditional East Asian Medicine as their primary modality for helping them live emotionally balanced lives after having tried medications without success, or if prescription medications just aren’t right for them.
What Does the Research Say?
A 2007 pilot study on PTSD randomized patients to either acupuncture treatment or cognitive behavioral therapy. Acupuncture provided positive treatment effects for PTSD with a decrease in symptoms by the end of their treatment. The positive effects were maintained at 3-month follow ups for both acupuncture and therapy(1). A 2015 meta-analysis on depression showed the effectiveness of acupuncture combined with medication. Using these combined therapies proved to have an early onset of action and were safe and well-tolerated when used together. Together, acupuncture with medication resulted in greater therapeutic effects than medication alone(2). Acupuncture was found to be helpful in treating major depressive disorder in pregnant women(3). One study done on students and staff at a large university found that acupuncture was successful in decreasing stress, and that the stress reduction lasted for at least 3 months after the completion of acupuncture treatment(4). Regarding anxiety disorders, studies analyzed in a 2018 review found that acupuncture enhances patients’ response to prescription anti-anxiety medications and that it may also reduce medication side effects(5).
References
1. Hollifield et al., Acupuncture for Posttraumatic Stress Disorder: A Randomized Controlled Pilot Trial. J Nerv Ment Dis. 2007 Jun;195(6):504-13.
2. Chan et al., The Benefit of Combined Acupuncture and Antidepressant Medication for Depression: A Systematic Review and Meta-Analysis. J Affect Disord. 2015 May 1;176:106-17. Epub 2015 Jan 28.
3. Sniezek D and Siddiqui I, Acupuncture for Treating Anxiety and Depression in Women: A Clinical Systematic Review. Med Acupunct. 2013 Jun; 25(3): 164–172.
4. Schroeder et al., Effectiveness of Acupuncture Therapy on Stress in a Large Urban College Population. J Acupunct Meridian Stud. 2017 Jun;10(3):165-170. Epub 2017 Jan 16.
5. Amorim et al., Acupuncture and Electroacupuncture for Anxiety Disorders: A Systematic Review of the Clinical Research. Complement Ther Clin Pract. 2018 May;31:31-37. Epub 2018 Jan 31.

Oriental Medicine Dietary Education and Consultations
Imagine this: you are relatively well-informed when it comes to food and nutrition. You feel that you have a well-balanced diet, with lots of fruits and vegetables, low fat yogurt, whole wheat bread, sugar-free drinks. You even make an effort to buy organic chicken. And yet, you are tired all the time. You suffer from indigestion. You have headaches. You sleep poorly. You are irritable. Despite regular exercise, you have a hard time losing weight. Sound familiar? It does to us, because we see many, many people, experiencing some variation of the above, walking into our clinic every week. The world of dietary and nutritional advice is full of contradicting opinions. The government tells you one thing, the CNN report with the “latest research” tells another story, and the newest dietary fad books say something else. Even one who makes Herculean efforts to become a well-educated consumer is often misled about what actually constitutes a healthy diet. This is why, day after day, we see people come to us, frustrated, seeking answers.
What does MHS have to offer that I can’t get somewhere else?
The practitioners at MHS have studied diet and nutrition for decades. We have a unique perspective on how food affects the body. We understand food from the Traditional East Asian Medicine perspective—for example, a woman who has very light menses and is trying to conceive should eat foods that build Blood such as liver, grass-fed beef, and beet roots. We also have extensive knowledge of nutrition from a scientific, research-driven perspective. For example, if someone comes to us seeking help for his deteriorating memory, we would assess his blood sugar and insulin regulation systems, re-balance these pathways, and subsequently improve his memory (1, 2). In the process, we would also be helping to decrease his risk for heart disease, diabetes, and hypertension; improve his work and athletic performance; and make it much easier for him to lose weight (3).
What does a Dietary Consultation entail?
We do a complete intake of your health history in order to understand your body and your nutritional needs. This is important because you are a unique person rather than a statistic. You are you, and your body may have very different needs from your friend who “followed that (fill in the blank) diet and lost 20 pounds.” After taking your history, we lay it out for you in simple terms. We explain the likely physiology of your body from an Oriental Medicine perspective, and what you need nutritionally. We give you breakfast, lunch, and dinner ideas. We help you explore different ways of eating that will benefit you. We give you a lot of dietary education—in the form of research studies, nutritional articles, and most importantly, food and recipe ideas—that will help you understand how food impacts your body and mind, and empower you to finally make the right choices for you. Then, we tell you to go and play with these new ideas for a while. For some people, one dietary consultation session is all that’s needed. They understand what needs to be done, enact the changes, lose the weight/pain/skin rashes/hot flashes, or gain energy/confidence/have a baby, and move on with their lives. Others may take a few weeks to make some changes, and return for a few more consultations as they explore, learn, and come up with questions on their journey to eating well.
I live far away. Can I still talk to someone about my diet?
Yes! We offer dietary educational information over the phone or online. Because of the detailed health history intake, the initial session may take up to an hour. Follow-up educational sessions, if needed, take 20-30 minutes.
Which conditions may benefit from changing my diet?
Allergies Andropause (male menopause) Arthritis Asthma Brain function, Focus/concentration, Memory loss Digestion: acid reflux, IBS Fatigue Fertility Food cravings Hair loss Headaches Kids: immune system, behavioral issues, developmental concerns Menstrual concerns: PMS, irregular/light/heavy/painful periods, anovulation Pain PCOS Perimenopause, Menopause Osteoporosis Skin rashes Sleep Weight loss/gain … and many, many others. Contact us or call 919-286-9595 to learn more.
- Correia SC, et al. Insulin signaling, glucose metabolism and mitochondria: major players in Alzheimer’s disease and diabetes interrelation. Brain Res. 2012 Jan 12 [Epub ahead of print]
- Bosco D, et al. Dementia is associated with Insulin Resistance in patients with Parkinson’s Disease. J Neurol Sci. 2012 Jan 20. [Epub ahead of print]
- Taubes, Gary. Good Calories, Bad Calories: Fats, Carbs, and the Controversial Science of Diet and Health. 2007. Alfred A. Knopf, New York.
Disclaimer: The content of the information presented during the online or phone sessions is for educational purposes only. The information and recommendations presented are not intended as a substitute for personalized medical advice. It is the sole responsibility of the user of this information to determine if the recommendations are appropriate for the user. Neither the practitioners or the clinic can be held liable for the information presented or any possible errors or omissions of such information. The information presented during these phone or online sessions should not be construed as a claim or representation that any type of food constitutes a cure, palliative or ameliorative. Foods described should be considered as adjunctive to other accepted conventional procedures deemed necessary by the user’s attending licensed physician. Foods presented during these sessions are not intended to diagnose, treat, cure, or prevent any disease.

Cancer Care
As Traditional Asian Medicine (TAM) becomes a more widely-accepted treatment modality, there is increasing evidence that it can assist cancer patients during their process of conventional treatment. Acupuncture and Chinese herbal therapy can alleviate many of the common side effects of radiation and chemotherapy, and significantly improve the quality of life for many patients.
What does the research show?
In the past few years, acupuncture and TAM have been the focus of increased interest and research funding. The National Institutes of Health (NIH) awarded grants for the first acupuncture trials in 1973. The Society of Acupuncture Research (SAR) promotes research in acupuncture and Chinese medicine, and was actively involved in the November 1997 Consensus Development Conference on Acupuncture, sponsored by the NIH. The panel concluded that, "...there is sufficient evidence of acupuncture's value to expand its use into conventional medicine and to encourage further studies of its physiology and clinical value." (1) The panel found considerable evidence that OM decreases nausea/vomiting during chemotherapy and relieves pain. (2) The American Cancer Society, on its website, states, "Acupuncture is an effective treatment for nausea caused by chemotherapy drugs and surgical anesthesia." (3,4,5)
Keith I. Block, MD, Medical/Scientific Director of the Institute for Integrative Cancer Care, states: "Serious exploration of alternative ways to improve the quality of life for persons undergoing cancer therapy represents a cornerstone as we face a new era in the treatment of this insidious disease. This can be accomplished by reducing pain, nausea and other debilitating 'side effects' - and most importantly, to give hope where it has perhaps diminished. As part of an integrative practice, I believe acupuncture has a solid and scientifically promising basis. Thus, continued investigation of acupuncture for clinical application and research is warranted in the area of cancer treatment.” (6)
W. Weiger, MD advises patients who seek complementary and alternative therapies for cancer: "Another potential role of acupuncture in patients with cancer is the palliation of chronic pain. Several case reports and series suggest that acupuncture may provide relief when conventional measures fail to control chronic pain resulting from underlying disease or conventional treatments (surgery or radiation). ... randomized controlled trials to date suggest that it is certainly reasonable to accept the use of acupuncture in conjunction with standard anti-emetics to control chemotherapy-related nausea and vomiting” (7,8,9,10,11,12,13,14,15).
Acupuncture has shown efficacy for advanced breast and lung cancer patients with dyspnea (difficulty breathing) when compared to a sham group. (16)  In a University of Pittsburgh Cancer Institute study, researchers received a grant of $1.2 million from the NIH to establish the role acupuncture may play in the treatment of patients with advanced colorectal cancer. "For many terminally ill colorectal cancer patients, their final months are marred by distressing physical and psychological symptoms," remarked Dr. Ellen Redinbaugh, the study's principal investigator. She added that the high hospitalization rates for such patients "indicate a clear need for new interventions to ameliorate their distress and promote their quality of life," and that "acupuncture holds promise as one such technique." (17)
In a University of Pittsburgh Cancer Institute study, researchers received a grant of $1.2 million from the NIH to establish the role acupuncture may play in the treatment of patients with advanced colorectal cancer. "For many terminally ill colorectal cancer patients, their final months are marred by distressing physical and psychological symptoms," remarked Dr. Ellen Redinbaugh, the study's principal investigator. She added that the high hospitalization rates for such patients "indicate a clear need for new interventions to ameliorate their distress and promote their quality of life," and that "acupuncture holds promise as one such technique." (17)
What is the role of Chinese herbs for cancer patients who are undergoing conventional treatments?
Chinese herbal medicine (CHM) also holds much promise in treating cancer patients. Like acupuncture, CHM can be used to relieve nausea in chemotherapy patients. Some patients are intolerant to the side-effects of standard anti-emetic or analgesic drugs, and can benefit significantly from acupuncture and herbal compounds combined. (19)
In a study with 182 cancer patients receiving chemotherapy, 98 were also given an herbal formula. It was modified to address issues like poor appetite, leukopenia, hemorrhaging of the digestive or respiratory tract, pain, jaundice, and nausea/vomiting. After 28 days, results observed for the group taking herbs in comparison to the group taking chemotherapy alone were reduced leukopenia and thrombocytopenia, improved appetite and increased body weight. Follow-up after five years revealed that recurrence and metastasis for the chemo/herb group was at 10 percent whereas for the chemo-alone group it was 35 percent. Mortality rates were at 8 percent for the chemo/herb group and 20 percent for the chemo-alone group. (19)
Several studies were done to test the effectiveness of radiotherapy when combined with Chinese herbal medicine. White blood and platelet counts tend to stay normal longer in radiation therapy patients with the inclusion of herbs, allowing patients to complete their prescribed courses of conventional treatments with increased potential for success. (20) Primary lung cancer patients were divided into two groups, one group received radiotherapy and CM combined, the other was treated with radiotherapy alone. In the combined group, 69 percent were able to complete their prescribed radiation course, while in the radiation alone group, only 31 percent could complete the course. Tumor circumference showed greater reduction using the combined approach. (20)
University of California researchers have found that Chinese herbs used with cancer patients “reduce the tumor load; prevent recurrence or formation of a new primary cancer; bolster the immune system; enhance the regulatory function of the endocrine system; protect the structure and function of internal organs and glands; strengthen the digestive system by improving absorption and metabolism; protect bone marrow and hematopoetic function; and prevent, control, and treat adverse side-effects caused by conventional treatments for cancer.” (22)
In the practice of OM, cancer is viewed as a part of a pattern of disharmony both stemming from and affecting the entire system (body-mind-spirit). OM views the imbalanced system as a potential amplifier of cellular aberrations. The main treatment strategy is to restore health by creating homeostasis within the system.
How much does it cost?
Patients can expect to receive 5 to 9 treatments over the course of three months in conjunction with ongoing chemotherapy and/or radiation therapy protocols at a cost of approximately $700-$1400. There is very little insurance coverage for acupuncture in North Carolina, though many of our patients pay for the cost of treatments with their flexible spending or health savings accounts.
How many treatments will I need?
Treatments are custom-tailored to fit each patient’s needs. Many patients find that acupuncture treatments so dramatically improve their response to standard therapy that they request an acupuncture treatment with each of their chemo/radiation sessions. For example, if a patient has chemo every Wednesday for 3 weeks in a row, she may have acupuncture every Tuesday during those 3 weeks, then skip acupuncture when she also has a week off from chemo. Other patients may find that one acupuncture treatment per two radiation sessions is sufficient support. During western medical treatment breaks, occasional acupuncture and daily herbal medicine may be used to build up your immune system, regulate digestion, and improve overall energy. The practitioners at MHS practitioners have a combined 50+ years of experience. We gladly work with you and your doctor to fit your needs, and help you have the best possible outcome.
References:
1. NIH Consensus Panel. Acupuncture. NIH Consensus Development Statement. Bethesda, MD, Nov 3-5, 1997
2. Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J R Soc Med. 1996. 89.303-311
3. American Cancer Society. [url=http://www.cancer.org]http://www.cancer.org[/url]
4. Shen J, et al. Electroacupuncture for Control of myeloablative chemotherapy induced Emesis: A randomized controlled trial. JAMA, 2000. 284(21):2755-2761
5. Beinfeld H, Korngold E. Chinese medicine and cancer care. Altern Ther Health Med. 2003;9(5).
6. Block KI. Acupuncture Complements Cancer Therapy. Acupuncture Today. February, 2003, Vol 04,(02)
7. Weiger W, Smith M, Boon H, et al. Advising patients who seek complementary and alternative therapies for cancer. Annals of Internal Medicine 2002;137:899-903.
8. King CR. Nonpharmacologic management of chemotherapy-induced nausea and vomiting. Oncol Nurs Forum 1997;24 (suppl. 7):41-48.
9. Rhodes VA, McDaniel RW. Measuring nausea, vomiting and retching. In: Frank-Stromberg M, Olsen SJ (eds.) Instruments for Clinic Health Care Res, 2nd ed. Boston, Jones & Bartlett,1997,pp.509-518.
10. de Aloysio D, Penacchioni P. Morning sickness control in early pregnancy by Neiguan point acupressure. Obstetrics and Gynecology 1992;80:852-854.
11. Belluomini J, et al. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study. Obstetrics and Gynecology 1994;84:245-248.
12. Fan CF, et al. Acupressure treatment for prevention of postoperative nausea and vomiting. Anesth Analgesia 1997;84:821-825.
13.Dibble SL, Chapman J, Mack KA, Shih A. Acupressure for nausea: results of a pilot study. Oncology Nursing Forum Feb 2000;27(1):41-7.
14. Pomeranz B. Acupuncture Analgesia-Basic Research, Stux G, Hammershlag R (eds), Clinical Acupuncture: Scientific Basis, Berlin:Springer-Verlag, 2001. pp. 1-29
15. Alimi D, et al. Analgesic effect of auricular acupuncture for cancer pain: A randomized, blinded controlled trial. J Clin Oncol, 2003. Vol 21(22):4120-4126.
16. Vickers AJ, et al. Acupuncture for dyspnea in advanced cancer: a randomized, placebo-controlled pilot trial. BMC Palliat Care, 2005 Aug 18,4:5.
17. Study examines acupuncture to alleviate symptoms for advanced colorectal cancer patients. EurekAlert news release, March 4, 2003.
18. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83
19. Wong R, Sagar CM, Sagar SM. Integration of Chinese medicine into supportive cancer care: a modern role for an ancient tradition. Cancer Treatment Reviews 2001;27:235-246.
20. Li Peiwen. Management of Cancer with Chinese Medicine. Donica Publishing, 2003. Distributed by Churchill and Livingstone. pp. 76-77. pp 79.
21. Zhang RJ, et al. Medicinal protection with Chinese herb compound against radiation damage. Aviat Space & Environ Med. 1990;61:729-31
22. Tagliaferri M. et al. Complementary and alternative medicine in early stage breast cancer. Seminars in Oncology, Vol 28, No 1(Feb), 2001:127.
Photo © Dagmar Ehling

Pain
Over 50 million people in the U.S. suffer from chronic pain. One in three people lose 20 hours of sleep per month due to pain. Although the quality, intensity, duration, and localization of pain is different for each individual, there are a few basic causes for most pain conditions:
Structural Imbalance: Scoliosis, uneven shoulder height, twisted hip girdle, tumors, or herniated disks can cause muscle tension or nerve pinching, and lead to pain.
Chronic Inflammation: Many factors such as inappropriate diet, blood sugar imbalance, lack of or incorrect exercise, repetitive stress (e.g. excessive computer work), and environmental pollution or toxins contribute to inflammation. Some patients even have an auto-immune condition in which pain is the main symptom. When a body’s tissues are inflamed, pain soon follows.
Stress: Sets off the body’s inflammatory cascade (see above), induces chronic muscle tension, and decreases one’s pain threshold. That means that the same level of pain actually feels more intense when one is in a stressed state, compared to when relaxed. 
Conventional treatments include pain medications, oral and injected steroids, antidepressants, physical therapy, and surgery. Some of these medications carry a significant risk of addiction, and others have strong side effects or are ineffective in the long-run.
Acupuncture is one of the most effective and non-invasive treatment modalities for addressing pain, and it is also among the best-documented complementary and alternative medicine (CAM) therapies in the scientific literature. A 2011 meta-analysis of CAM therapies showed that acupuncture was significantly more effective at relieving pain as compared to placebo, physical therapy, or usual care (1).
Studies also suggest that acupuncture can be more effective than conventional therapies for post-cecarean pain (2); patients who received acupuncture for their low back pain were less likely to seek physician services for the low back pain than those patients who had not received acupuncture (3); acupuncture treatment significantly improved all measurable outcomes in patients who had migraine, episodic, and chronic tension-type headaches (4)… The studies go on and on.
Pain and its associated health problems are among the top three reasons for patients seeking care at MHS. We address pain in a comprehensive manner.
The various Acupuncture styles practiced at MHS target specific types of pain conditions. Often, patients experience pain relief during treatment that is both significant and long-lasting. Acupuncture treatments also help to regulate the immune system, promote healthy circulation patterns, and decrease the stress response, all of which help to address pain at the root level.
We provide Dietary Counseling to give your unique constitution a nutrient-dense and anti-inflammatory diet.
If needed, we use Herbal and Nutritional Supplementation to further decrease inflammation, via improved fundamental biological processes such as blood sugar regulation, hormonal balance, and immune system and organ system function.
A combination of the above therapies expedites results. When applied appropriately, patients experience rapid and lasting improvements that significantly improve their quality of life.
References
1. Frulan AD, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med. 2012;2012:953139. Epub 2011 Nov 24.
2. Xu J, and Mackenzie IZ. The current use of acupuncture during pregnancy and childbirth. Curr Opin Obstet Gynecol. 2012 Jan 13.
3. Moritz S et al. Reduced health resource use after acupuncture for low-back pain. J Altern Complement Med. 2011 Nov;17(11):1015-9. Epub 2011 Nov 9.
4. Melchart D et al. Acupuncture for chronic headaches--an epidemiological study. Headache. 2006 Apr;46(4):632-41.
5. Mannheimer et al. Meta-analysis: acupuncture for low back pain. Ann Intern Med 2005;142:651
6. Molsberger AF et al. Does acupuncture improve the orthopedic management of chronic low back pain? – A randomized, blinded, controlled trial with 3 months follow-up. Pain 2002;99:579-587
7. Berman BM et al. Effectiveness of Acupuncture as Adjunctive Therapy in Osteoarthritis of the Knee. A randomized controlled trial. Ann Intern Med 2004;141:901-910
8. Hsieh LL et al. Treatment of low back pain by acupressure and physical therapy: randomised controlled trial. BMJ 2006;332:696
9. Carlsson C, Sjölund B. Acupuncture for chronic low back pain: a randomized placebo-controlled study with long-term follow-up. Clinic J Pain; 2001;17(4): 296-305.
10. Vickers AJ et al. Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis. Health Technol Assess 2004;294:2118
11. Witt C et al. Acupuncture in patients with osteoarthritis of the knee: a randomized controlled trial. Lancet 2005;366:136
12. Vas J et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomized controlled trial. BMJ 2004;329:1216
13. Sprott H, Franke S, Kluge H, et al. Pain treatment of fibromyalgia by acupuncture. Rheumatol Int 1998;18(1):35-6.
14. Assefi NP, Sherman KJ, Jacobsen C, et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med July 5, 2005;143(1):10-9.
15. Berman BM, Swyers JP, Ezzo J. The evidence for acupuncture as a treatment for rheumatologic conditions. Rheum Dis Clin North Am Feb 2000;26(1):103-15, ix-x.
16. Ho KY, Jones L, Gan TJ. The effect of cultural background on the usage of complementary and alternative medicine for chronic pain management. Pain Physician. 2009 May-Jun;12(3):685-8. (2009)
17. Sun Y, Gan TJ, Dubose JW, Habib AS. Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials. Br J Anaesth. 2008 Aug;101(2):151-60. (2008)

Andropause
The term “Andropause” is to men what “Menopause” is to women. Andropause is a gradual but consistent decline in the sex hormones of middle-aged men. Andropause is a very real health phenomenon affecting millions of men in the world, but it is not officially recognized by the World Health Organization. The medical profession and public awareness of andropause today are similar to their ignorance of menopause a few decades ago. As a result, men suffering from the effects of andropause are unable to find much-needed help and guidance (1).
Andropause plays out over a longer period of time than menopause. Hormonal shifts such as a decline in testosterone levels begin taking place starting in a man’s mid-30s, and continue until his 50s or later. These shifts, taking place over decades, mean that the day-to-day changes in men are subtle. By the time symptoms are evident—showing up as loss of muscle mass, decreased athletic performance, poor mental function, or diminished sex drive—a slow sapping of vitality and vigor have occurred, and the pathology is already in place.  Andropause is best defined as a state in which males cease to be androgen, or male hormone, dominant. In other words, the male body and brain, which should operate predominantly on androgens, no longer do. Thus, they fall under the influence of the relatively dominant, increased estrogen levels.
Andropause is best defined as a state in which males cease to be androgen, or male hormone, dominant. In other words, the male body and brain, which should operate predominantly on androgens, no longer do. Thus, they fall under the influence of the relatively dominant, increased estrogen levels.
Of the ten most common causes of death in males, five are directly related to this decline in androgen dominance. These five causes of death, heart disease, stroke, diabetes, suicide (depression) and Alzheimer’s disease are major players in health risks for men, and proper management of men’s health in their middle years can play a significant role in prevention and treatment of these disease patterns.
Benign prostatic hyperplasia (BPH) is a very common andropause disorder, and most men wrestle with this complaint at some point during their later lives. All men will have increased proliferation of their prostate tissues; nearly 60% of men between 40 and 59 have an enlarged prostate. So the question for men is not “How do I avoid prostate enlargement?” but “How do I keep an enlarged prostate from causing me problems?” The answer lies in good management of andropause.
The gradual presentation of andropause makes many men accept their symptoms as part of “normal aging,” which prevents them from seeking care for a decline that can respond well to intervention.
How does Western Medicine Treat Andropause?
Conventional medical treatment typically consists of medications to treat presenting symptoms such as high cholesterol, diabetes, depression, or erectile dysfunction. Fully 62% of the top 50 most prescribed drugs relate to the pathophysiology and metabolic effects of andropause. For BPH, drug treatments, transurethral microwave radiation (heating the prostate to at least 111 degrees Fahrenheit), transurethral needle ablation, high intensity ultrasound and surgery are standard interventions.
How does MHS manage Andropause?
There are many contributing factors that increase risk for andropause symptoms. Inflammation, insulin resistance or diabetes, low testosterone, obesity, declining mental function, and impaired circulation all work in an interrelated fashion to cause a shift from androgen dominance.
Supporting brain function, specifically acetylcholine activity, increasing blood flow to the brain and peripheral vascular system (erectile dysfunction is generally a vascular, neurologic or psychogenic issue, not an endocrine problem), regulating blood sugar metabolism, controlling inflammation, and enhancing digestion are among the goals of therapy at MHS.
A thorough health history intake, physical examination according to Traditional East Asian Medicine principles, and possibly looking at laboratory blood tests will help to make clear the priorities for each man. Treatment is usually multi-faceted, involving:
Acupuncture to improve circulation and clarify a Traditional East Asian medical diagnosis, which will aid in refining an intervention for more rapid and patient-specific results;
Dietary counseling to improve blood sugar metabolism, help reduce inflammation, support energy production, and help achieve optimal weight maintenance;
Herbal and nutritional supplementation can target specific metabolic pathways and speed the process of balancing blood sugar metabolism, the endocrine system, brain function and digestion.
As a population, men tend to be poor at self-care, and are often reluctant to seek medical care whether it is from a conventional or a complementary provider. But more and more men are realizing the benefits of preventive care. As men live longer, they find it increasingly important to maintain optimal energy, acute mental function, balanced emotional states, and high physical strength and stamina.
Tackling the health issues of andropause head-on, and addressing the multiple systems involved in the aging process, significantly reduces the risk of many age-related diseases while making a full and vital life, long into “old age”, a reality.
Selected studies of interest:
Harrison J. Talking about my generation: a state of the art review of health information for men in the andropause. Health Info Libr J. 2011 Sep;28(3):161-70.
Wang X, Stocco DM. The decline in testosterone biosynthesis during male aging: a consequence of multiple alterations. Mol Cell Endocrinonol. 2005 Jun 30:238(1-2):1-7. This study discusses age related increases in COX 2 enzymes (inflammatory enzymes inhibited by NSAIDS) which may cause a reduction in testosterone concentrations.
Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat Rev Endocrinol. 2009 Dec;5(12):673-81. Epub 2009 Oct 27. “. . . central obesity and insulin resistance are acknowledged as important causative factors (in metabolic syndrome). The amount of visceral adipose tissue is inversely associated with testosterone concentrations. Low testosterone levels are associated with insulin resistance and high testosterone concentrations are linked with insulin sensitivity.”
Carreau S, et al. The Promoter(s) of the aromatase gene in male testicular cells. Reprod Bil. 2004 Mar;4(1):23-34. “In human adipose tissue, the primary promoter of aromatase gene expression (is). . , driven by class I cytokines IL-6 and TNF alpha” (this means that testosterones will drop and estrogen levels will rise, a bad scenario for males).
Gouras GK, et al. Testosterone reduces neuronal secretion of Alzheimer’s B-amyloid peptides. PNAS. 2000;97(3):1202-1205.
Moffat SD. Effects of testosterone on cognitive brain aging in elderly men. Ann NY Acad Sci. 2005;1055:80-92.
Giltav EJ, Haider A, Saad F, Gooren LJ. C-reactive protein levels and aging male symptoms in hypogonadal men treated with testosterone supplementation. Andrologia, 2008 Dec;40(6):398-400.

Autoimmune
It is estimated that in the U.S. alone:
- 16 million people, or over 5% of the population, have autoimmune thyroid disorders such as Hashimoto’s or Graves’ disease.
- Nearly 4 million people have been diagnosed with rheumatoid arthritis.
- 7 million people, or about 2-3% of the population, have psoriasis.
- 1.5 million people have Crohn’s disease or ulcerative colitis.
The above conditions are all classified as “Autoimmune Disorders,” an umbrella diagnosis that includes over 100 conditions.  Autoimmune disorders stem from chronic inflammatory processes that eventually prompt a person’s immune system to attack his or her own body tissues. Patients with autoimmune diseases have antibodies in their blood that target the destruction of specific body tissues such as the joints, skin, connective tissue, glands, and others. Autoimmune disorders can be minor annoyances, with mild symptoms involving one area of the body. Or they can be severe, affecting many body systems, and cause chronic and debilitating health issues.
Autoimmune disorders stem from chronic inflammatory processes that eventually prompt a person’s immune system to attack his or her own body tissues. Patients with autoimmune diseases have antibodies in their blood that target the destruction of specific body tissues such as the joints, skin, connective tissue, glands, and others. Autoimmune disorders can be minor annoyances, with mild symptoms involving one area of the body. Or they can be severe, affecting many body systems, and cause chronic and debilitating health issues.
How does Western Medicine Treat Autoimmune Disorders?
Conventional medical treatment typically consists of immune-suppressant medications such as steroids or chemotherapy agents. Long-term usage of such medications results in devastating side effects such as chronic infections, hypertension, gastric ulcers, and even liver and kidney damage.
How does MHS Treat Autoimmune Disorders?
The practitioners at MHS have extensive training in the management of autoimmune disorders. It is important to understand that once you have an autoimmune disorder, you will always have it. However, with proper management, you do not always have to suffer from it. Autoimmune disorders can have states of flare-up and remission, which are linked to the amount of inflammation present in the body.
Decreasing inflammation is therefore paramount in successful management of autoimmune disorders, and the practitioners at MHS approach this with a combination of strategies:
Acupuncture to regulate the immune system, promote healthy circulation patterns, decrease the stress and inflammatory response, and alleviate pain;
Dietary counseling to target your unique constitution, and provide an anti-inflammatory diet that dampens the immune system’s hyperactive, damaging activities, and promotes its healing properties;
Herbal and nutritional supplementation to improve your fundamental biological processes such as blood sugar regulation, hormonal and neurotransmitter balance, and immune system modulation which result in decreased inflammation.
We have numerous patients with autoimmune disorders who were overmedicated, poorly managed, suffering immensely, and came to MHS as a “last resort”. These patients span a spectrum of many conditions—Hashimoto’s, rheumatoid arthritis, psoriasis, multiple sclerosis, Celiac disease, on and on…
Most of the patients who follow through with our treatment regiment have significantly improved their health. They are empowered because they know how to avoid the triggers of their flare-ups. Or, if they have an unavoidable stressor that does trigger a flare-up, these patients have the tools to manage it and return to a healthy, asymptomatic state as quickly as possible. With proper management, our autoimmune patients experience a high quality of life.
Selected studies of interest:
Tewthanorn K, et al. Correlation of lipid peroxidation and glutathione levels with severity of systemic lupus erythematosus: a pilot study from single center: J Pharm Pharm Sci. 2008;11(3):30-4
Tada-Oikawa S, et al. Critical role of hydrogen peroxide in the differential susceptibility of Th1 and Th2 cells to tributyltin-induced apoptosis: Biochem Parmacol. 208 Jan 15;75(2):555-61. Epub 2007 Sep 18
Won HY, et al. Glutathione Peroxidase 1 Deficiency Attenuates Allergen-Induced Airway Inflammation by Suppressing Th2 and Th17 Cell Development: Antioxid Redox Signal. 2010 Jun 6
Yan Z, et al. Extracellular redox modulation by regulatory T-cells: Nat Chem Biol. 2009 Oct,5(10):721-3. Epub 2009 Aug 30.
Niedbala W, et al. Role of nitric oxide in the regulation of T-cell functions. Ann Rheum Dis. 2006 Nov;65 Suppl 3:iii37-40
Mendez II, et al. Immunoregulatory role of nitric oxide in Kilham rat virus-induced autoimmune diabetes in DR-BB rats: J Immunol. 2004 Jul15;173(2):1327-35
Miljkovic D, Trajkovic V. Inducible nitric oxide synthase activation by interleukin-17: Cytokine Growth Factor Rev. 2004 Feb;15(1):21-32. Review.
Shi FD, et al. Control of the autoimmune response by type 2 nitric oxide synthase: J Immunol. 2001 Sep1;167(3):3000-6
Rubio-Tapia A, et al. Increased prevalence and mortality in undiagnosed Celiac disease: Gastroenterology. 2009 Jul;137(1):88-93. Epub 2009 Apr 10

Food Sensitivities
Do you have a rapid and severe reaction to walnuts? If so, you probably have a food allergy. Or, do you feel bloated and have congestion the day after you eat ice cream? If so, that points toward a food intolerance. "Allergy” implies an IgE-mediated immune response that can be as extreme as severe anaphylaxis, whereas “intolerance” points to milder negative reactions, generally mediated by IgA and IgG.
Both food allergies and intolerances are on the rise, but the delayed and less-specific symptoms of food intolerances make it more confusing, pervasive, and one of the most under-addressed issues in healthcare today. Common foods associated with food intolerance include gluten and dairy. Clinically, at MHS, we have seen a spectacular rise in gluten-associated conditions in the last decade. This observation is backed by scientific studies, which have found that in the last 50 years, the incidence of celiac disease has increased from 1 in 700 people to 1 in 100 (1), and these increases are not merely due to higher diagnostic rates (2).
If one has a food intolerance, identifying and eliminating the problematic foods are an absolutely essential step in order to achieve health (3). For example, in a person who has gluten intolerance, every time that she eats gluten-containing foods (which includes bread, cereal, snacks bars, and almost all processed foods), her body mounts an immune response to the gluten, creating an inflammatory cascade that could elicit indigestion, pain, brain fog, neurological symptoms, thyroid imbalance, or even affect hormonal balance and fertility (4, 5).  Common symptoms of food sensitivities include irritability, headaches, migraines, bloating, fatigue, aching joints, diarrhea, high blood pressure, and focus problems (6).
Common symptoms of food sensitivities include irritability, headaches, migraines, bloating, fatigue, aching joints, diarrhea, high blood pressure, and focus problems (6).
We at MHS are trained to recognize the patterns that could be associated with specific food intolerances. Once recognized and eliminated, we then work to heal the gut and systemic damage that most likely occurred during the years when one consumed foods that their immune system rejected. We provide careful guidance in helping the patient navigate the dietary challenges that come with a food inventory overhaul.
References:
1. Rubio-Tapia A, et al. Increased prevalence and mortality in undiagnosed Celiac disease: Gastroenterology. 2009 Jul;137(1):88-93. Epub 2009 Apr 10
2. Rubio-Tapia A, Murray JA. Celiac disease: Curr Opin Gastroenterol. 2010 Mar;26(2):116-22.
3. Duggan JM. Celiac disease: the great imitator: Med J. Aust. 2004 May 17;180(10):524-6. Review.
4. Hadjivassiliou M. Immune-mediated acquired ataxias. Handb. Clin. Neurol. 2012; 103:189-99.
5. Hadjivassiliou M, et al. Gluten sensitivity: from gut to brain. Lancet Neurol. 2010 Mar; 9(3):318-30.
6. Vojdani A. Lecture notes. Neuroimmunology, sponsored by Carrick Institute. 2012.

Allergies
According to the NIH, allergic diseases affect more than 50 million Americans. Environmental allergies are very common, with over 17 million new diagnosed cases of hay fever annually in the U.S. They result from a hypersensitivity of the immune system, which reacts to particulates or allergens including pollen, dust, molds, dander and environmental toxins. An inflammatory response occurs, releasing histamines and leukotrienes, which cause sneezing, itchy and watery eyes, nasal congestion, headache, runny nose, and possibly sinusitis.
What Is The Western Treatment?
Western Medicine tends to treat allergies in three ways. The first approach involves the use of anti-histamines or anti-leukotrienes, either over the counter (i.e. claritin, benadryl) or by prescription (i.e. Allegra, Singulair). The second type of treatment involves the use of nasal steroids such as nasonex or flonase to reduce swelling and inflammation from the histamine response. Finally, some are treated with injections to the particular allergen to decrease the body’s histamine response. These therapies can often be problematic, carrying the side effects of drowsiness, dry mouth, sleep interference, or, in the case of the injections, a 3-5 year regimen that is time-consuming, and not feasible nor effective for everyone.
What is the Traditional East Asian Medicine Treatment?
 Traditional East Asian Medicine employs a combination of acupuncture, herbal remedies, and proper nutrition in order to re-balance the immune system. A randomized controlled study on persistent allergic rhinitis in pediatric patients compared true vs. sham acupuncture in its treatment. The authors concluded that true acupuncture was more effective than sham acupuncture in decreasing the symptom scores for persistent allergic rhinitis and increasing the symptom-free days. (1)
Traditional East Asian Medicine employs a combination of acupuncture, herbal remedies, and proper nutrition in order to re-balance the immune system. A randomized controlled study on persistent allergic rhinitis in pediatric patients compared true vs. sham acupuncture in its treatment. The authors concluded that true acupuncture was more effective than sham acupuncture in decreasing the symptom scores for persistent allergic rhinitis and increasing the symptom-free days. (1)
Acupuncture and Chinese herbal medicine have been shown to be effective in treating allergies by stimulating and strengthening the body’s immune system, regulating the immune response and alleviating the signs and symptoms of allergic rhinitis. A randomized controlled trial from 2004 studied 52 patients with chronic seasonal allergic rhinitis. The control group received acupuncture to non-acupuncture or sham points and a non-specific herbal decoction. The study group received a semi-standardized treatment of acupuncture and a prescribed Chinese herbal decoction. The results showed an 85% improvement in the study group and only a 40% improvement in the control group. The study group also showed a significant improvement after treatment on the VAS (visual analogue scale) and the rhinitis quality of life questionnaire. (2)
Treatments for environmental allergies address each individual’s needs depending on what signs and symptoms are present. Studies show that treatments are more effective when patients take herbs specifically for their needs in addition to acupuncture (3). This also cuts down the overall cost of treatment, as the patient gets daily support between the acupuncture treatments, thus requiring fewer acupuncture treatments.
References:
1. Daniel K. Ng, FRCP, et al. A Double-Blind, Randomized, Placebo-Controlled Trial of Acupuncture for the Treatment of Childhood Persistent Allergic Rhinitis. Pediatrics. Vol. 114 No. 5 November 2004, pp. 1242-1247
2. Brinkhaus, B., et al. Acupuncture and Chinese herbal Medicine in the treatment of patients with seasonal allergic rhinitis: a randomized-controlled clinical trial. Allergy, 2004; 59 (9), 953-960.
3. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83

Breast pain associated with lactation
 Beginning in 2004, the practitioners of Meridian Health Solutions (MHS) have been working in conjunction with the lactation consultants at UNC-Chapel Hill to study the use of acupuncture in treating breast pain associated with lactation. For the purpose of this study, all patients referred to MHS have received western or conventional-medicine treatment for a minimum of one month without positive results. Given that the lactation consultants at UNC are among the best in the region, these referrals are generally considered to be the most recalcitrant and difficult-to-treat cases.
Beginning in 2004, the practitioners of Meridian Health Solutions (MHS) have been working in conjunction with the lactation consultants at UNC-Chapel Hill to study the use of acupuncture in treating breast pain associated with lactation. For the purpose of this study, all patients referred to MHS have received western or conventional-medicine treatment for a minimum of one month without positive results. Given that the lactation consultants at UNC are among the best in the region, these referrals are generally considered to be the most recalcitrant and difficult-to-treat cases.
Our in-house data show that we're able to help reduce lactation pain in the majority of the cases we see, with most patients experiencing immediate pain reduction during the first treatment. Patients are properly draped during these treatments with no needles ever inserted into their breasts, making this a safe and comfortable treatment process. We give patients acupressure points they can stimulate at home either with massage or heat, which is easy to do, lengthens the benefits of the treatments, and reduces the number of treatments they require.
As clinicians who care deeply about the health of new mothers and babies, we are so glad to provide treatments that quickly, safely, and effectively reduce lactation pain, since healthy breastfeeding is so important for the short and long term health of the mother and baby. As a result of ongoing benefits to the patients, we're still getting regular referrals from the UNC-Chapel Hill lactation consultants almost 20 years after initiating the study!
Traditional East Asian Medicine Treatment Strategies
One of Traditional East Asian medicine’s foundational principles emphasizes that every individual is unique. That is, even if two people present with similar complaints, the cause of illness for one person almost certainly differs from that of the other. Therefore every person’s course of treatment must be individually-tailored to suit their particular need, including when treating lactation pain.
Acupuncture is the insertion of sterile, thin needles into specific sites on the body. Pain is usually caused by what Chinese medicine calls “stagnation,” therefore, the treatment is aimed toward inserting needles at sites that would open the energy channels and remove energy stagnation. When treating lactation-associated breast pain, acupuncture opens the corresponding channels, thereby reducing the pain. Often, the pain reduction/elimination is immediate upon insertion of the appropriate needles.
Chinese Herbal Medicine (CHM) is a science and art supported by at least 2,000 years of empirical practice. Medical practitioners have prescribed herbs for post-partum complaints for centuries. This form of therapy can be useful for lactating women as well, with unique herbal formulas recommended for specific conditions.
Nutrition is an essential component of good general health, and is an especially important aspect for those with plugged ducts associated with lactation. Understanding a mother’s and her baby’s dietary and nutritional needs provides the framework for implementing specific, effective dietary changes. The suggested changes usually involve introducing nutritious and delicious foods into the diet. Often, simple dietary changes make a profound difference within one week.
Western Medicine’s Approach
Western medicine can offer antibiotic or antifungal medications in cases of bacterial and fungal infections in a lactating woman. These medications can be oral or topical. However, a common conundrum is that when a woman has a bacterial infection, the antibiotics that treat the infection often are the cause for a consequent fungal infection. In the absence of identifiable infection, lactation consultants will work with a nursing mother to identify possible causes of lactation pain, such as vasospasm of the areola, improper breastfeeding positioning, or poor latch-on by the infant. Remedies for these conditions may include warm compresses, dietary supplements, and correcting the infant's latch.
What Can I Expect During a Session?
During the initial visit we discuss your medical history, your baby’s nursing history, take a careful look at your dietary habits, and perform a physical examination. The physical examination consists of checking the pulse on your wrists, looking at the tongue and performing diagnostic palpations around the abdomen and neck. We may ask you to find the most painful area on your breast(s) yourself while we palpate other areas on your body with the intention of releasing the pain in your breasts. The palpations offer further insights into the exact nature of your situation. The breast itself is never needled. The overall treatment plan typically consists of some combination of acupuncture, acupressure homework, custom-tailored herbal medicine, nutritional changes, and stress reduction techniques.
References
1. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83
2. Neri I, et al. Acupuncture treatment as breastfeeding support: preliminary data. J Altern Complement Med 2011 Feb;17(2):133-7. Epub 2011 Feb 8.
3. KvistLJ, et al. A randomised-controlled trial in Sweden of acupuncture and care interventions for the relief of inflammatory symptoms of the breast during lactation. Midwifery. 2007 Jun;23(2):184-95. Epub 2006 Oct 18.

Menopause
More than 1 million U.S. women enter menopause each year. A woman is defined as “menopausal” when she hasn’t had a period for one year. The average age of becoming menopausal is between 48-55 years old. One hundred years ago, not many women lived past her early 50s, and so being in a menopausal state was a rarity. With our increasing life expectancy, many of today’s women can be in their menopausal lifestage for more than thirty years.
Perimenopause is the transitional period preceding menopause, when a woman’s menstrual cycles start becoming more irregular. During the perimenopause transition, many women experience symptoms such as hot flashes, insomnia, irritability, mood swings, night sweats, lowered libido, depression, foggy brain, and general body pain.
Physical change may include vaginal atrophy, incontinence, and skin atrophy. The incidence of certain disease states such as cardiovascular disease, osteoporosis, dementia (Alzheimer-like), and cancer increases.
Every now and then, we meet a woman who fares the perimenopause-to-menopause transition with extreme ease and grace. She may experience a gradual lengthening in the time between her cycles, until one day, she has no more periods. She is able to carry on with life in the same way as before—with steady energy, strength, and mental clarity. The only difference is that she no longer needs to be bothered with a monthly period.
The majority of women, though, experience something more difficult. In our clinic, we have seen the difficulties range from moderately uncomfortable hot flashes to severe, drenching sweats paired with insomnia, anxiety, exhaustion, severe joint pain, body rashes, and even the onset of autoimmune disorders.
How do we reconcile these two above realities? How can the same term—menopause—even be applied to such different pictures? It is important to understand that menopause is a process. Though we now lead lives of instant gratification, our bodies respond to the days and years of nourishment (or lack thereof!) that precede the here and now. How you nurture your body before the perimenopausal transition—your diet, exercise, state of mind, stress levels—will always be reflected in how you handle perimenopause and menopause.
The practitioners at MHS have an advanced and comprehensive understanding of the energetics, physiology, and neuroimmunology underpinning the menopausal process. Though it may not be explicitly stated, when we work with women in their 30s and 40s (and even when we see a little 2-year-old girl here in the clinic), we are working to build the foundations for a balanced hormonal system that will one day be invaluable during their menopausal years.
And when a new patient comes to us, around her perimenopausal time, with her life seemingly falling apart from all the symptoms that are “suddenly” upon her, we use our training to quickly hone in on the root(s) of the imbalance, begin the process of nourishment and repair, so that she can move forward in a positive way. 
For menopausal health issues, we employ 3 main treatment strategies:
Acupuncture to promote healthy circulation patterns, reduce inflammation, balance the immune system, decrease the stress response, and alleviate pain;
Dietary counseling with a focus on nutrient-dense foods that promote a strong immune system, balance blood sugar levels, optimize body composition and weight, and promote overall health;
Herbal and nutritional supplementation to balance hormones, regulate menstrual cycles, stabilize blood sugar, promote quality rest, and enhance mental-emotional well-being.
References:
1. Kraft K, Coulon S. Postmenopausal High Blood Pressure: Standardized Acupuncture can reduce postmenopausal complaints, but does not alter blood pressure. Forsch Komplementärmed. 1999: Apr;6(2):74-9.
2. Wyon Y, et al. Menopausal Hot Flashes: Significant decrease in numbers of hot flashes in electro-acupuncture and in superficial needling acupuncture group. Lakartidningen. 1994: Jun 8;91(23):2318-22; and Wyon Y, et al. 1995 Menopause 2:3-12.

Women’s Health
Women’s health issues are commonly thought of as isolated conditions, without connection to the rest of the body, and conventional treatments often reflect as such. For example, heavy periods can lead to surgical removal of a uterus, and menopausal symptoms are treated with antidepressants or hormone replacement therapy.
Very rarely is a woman asked the question, “How are these symptoms a reflection of your overall physical health and mental state?” We ask that question at MHS, where gynecological issues provide a window into a woman’s general well-being.
We incorporate mind and body in diagnosis and treatment of women’s issues, with great success in achieving health for the whole person. Here we list two commonly-seen examples.
Polycystic Ovarian Syndrome (PCOS) is characterized by lack of mature follicle development in the ovaries, irregular or no ovulation and periods, infertility, excessive growth of facial and body hair, and weight gain. PCOS is caused by insulin resistance. Conventional medicine manages PCOS symptoms with diabetes medications or the birth control pill.
Applying our understanding of the underlying physiology, our treatment approach for PCOS successfully reduces insulin resistance, promotes weight loss, regulates periods and ovulation, and improves fertility.
Endometriosis is growth of uterine (endometrial) tissue outside of the uterus, often leading to pelvic pain, abdominal adhesions, very heavy periods, and may be implicated in infertility. Conventional treatments include hormonal therapies, pain relievers, and surgical removal of extra-uterine endometrial tissue.
Our treatments support the normalization of endometrial tissue, rebalance circulation, alleviate pain, and promote fertility.
For the above and most other women’s health issues, we employ 3 main treatment strategies: 
Acupuncture to promote healthy circulation patterns, balance the immune system, decrease the stress response, and alleviate pain;
Dietary counseling with a focus on nutrient-dense foods that provide optimal reproductive and overall health;
Herbal and nutritional supplementation to balance hormones, regulate menstrual cycles, stabilize blood sugars, and enhance mental-emotional well-being.
Common Women’s Health Conditions Treated at MHS:
Preconception / fertility Acupuncture to enhance IVF outcomes
Miscarriage Prevention
Prenatal / Postpartum conditions
Labor preparation
Lactation support
Anovulation (absence of ovulation)
Amenorrhea (absence of periods)
Dysmenorrhea (painful periods)
Endometriosis
Normalizing cycles after stopping hormonal contraceptives
Premenstrual syndrome
PCOS / irregular cycles
Ovarian cysts
Uterine fibroids
Fibrocystic breasts
… And many, many more.
References:
1. Ternov K, et al. Pain relief during Labor. Analgesic use less in Acupuncture group vs Standard care group: Acupunct Electrother Res. 1998;23(1):19-26]
2. de Aloysio D, Penacchioni P. Morning sickness control in early pregnancy by Neiguan point acupressure. Obstetrics and Gynecology 1992;80:852-854.
3. Belluomini J, et al. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study. Obstetrics and Gynecology 1994;84:245-248.
4. Riordan J, Nichols F: A descriptive study of lactation mastitis in long-term breastfeeding women. Journal of Human Lactation 6:53-8, 1990
5. Walker EM, Rodriguez AI, Kohn B, et al. Acupuncture Versus Venlafaxine for the Management of Vasomotor Symptoms in Patients With Hormone Receptor–Positive Breast Cancer: A Randomized Controlled Trial. J Clinic Oncology, 10.1200/JCO.2009.23.5150.
6. Singh BB, Berman BM, Simpson RL, Annechild A: Incidence of premenstrual syndrome and remedy usage – a national probability sample study. Alternative Therapies in Health and Medicine 1998; 4:75-79.
7. Oleson T, Flocco W: Randomized controlled study of premenstrual symptoms treated with ear, hand, and foot reflexology. Obstetrics and Gynecology 1993; 82:906-911.
8. Helms JM: Acupuncture for the management of primary dysmenorrhea. Obstetrics and Gynecology 1987; 69:51-56.
9. Lewers D, Clelland JA, Jackson JR, Varner RE, Bergman J: Transcutaneous electrical nerve stimulation in the relief of primary dysmenorrhea. Physical Therapy 1989; 69:3-9.
10. Steinberger A: The treatment of dysmenorrhea by acupuncture. American Journal of Chinese Medicine 1981; 9:57-60.

Fertility
We have helped bring hundreds of healthy babies into this world. Sometimes it’s a breeze! We nourish the right bodies in the right ways at the right time, and the perfect baby arrives.
Other times the process is harder: would-be parent(s) may come to us with years-long health challenges that have prevented them from conceiving. We work with each person to address their unique needs, for months or sometimes even a couple years, until step by step they restore their fertility, the right day comes, and the perfect baby arrives.
Anyone on the fertility journey already knows the news isn’t good: Infertility is a shockingly common problem in our modern world, affecting more than 20% of people in the U.S. who are trying to conceive (www.cdc.gov).
The problems can stem from multiple sources, both male and female: sperm count or quality, varicoceles, ejaculations disorders; ovary, uterine, and cervical problems, endometriosis, PCOS; auto-immune disease and diabetes frequently complicate fertility problems.
It’s a lot to navigate, and you’re supposed to do it while keeping your cool, because stress is bad for fertility!? How does one do that? This is where we get to help.
How can Traditional East Asian Medicine (TEAM) enhance Fertility?
Traditional East Asian Medicine (TEAM) has long been known to treat both female and male infertility (Zhu et al 2018, Feng et al 2021). Fertility treatments at Meridian Health Solutions aim to create healthy sperm, healthy eggs, a welcoming womb environment, and an open heart.
Treatments use a combination of herbal medicine, acupuncture, and diet, which are tailored to each person’s unique needs. We counsel people on incorporating nutrient-dense “fertility foods” used by many traditional cultures. These tools reset you into overall better health so your fertility journey becomes an easier route.
Specifically, they improve blood flow to the reproductive organs, so the sperm, eggs, and endometrial lining grow into healthy terrain for creating and sustaining life. It’s our goal not only to help you have a child, but to have an extremely healthy child!
What if I have a medical issue and have to use ART?
Some medical causes of infertility can benefit greatly from Western medicine’s assisted reproductive technology (ART). ART is often a costly and invasive therapy, though it can help people have a baby when it would otherwise be impossible.
Many high-performing ART clinics have chosen to include Acupuncture as a part of their patients’ process, to help improve success rates.
Meridian Health Solutions practitioners can provide guidance and comfort through your ART process. We offer treatments to reduce side effects and improve outcomes. Reproductive endocrinologists even ask us to perform specific treatments to aid their process. For example, we can help one’s uterus less likely to spasm during egg retrieval so more eggs are available; or we can help to improve uterine lining quality for successful embryo transfer and implantation.
Most importantly, we help you manage this stressful time with information and tools that support your whole-person health.
What types of fertility-related medical issues can acupuncture help with?
- High FSH
- Difficulty with implantation/conception
- Recurrent miscarriage
- Polycystic Ovarian Syndrome/PCOS
- Thin uterine lining
- Sperm count, morphology, motility
- Side effects from Assisted Reproductive Technology/ART
- Poor response to IUI/IVF
How many sessions do I need?
Although not required, we suggest you begin therapy at least three months prior to trying to conceive, either naturally or with ART. Sperm development takes 70-90 days from start to finish; dormant egg cells take a comparable amount of time to mature; and it may take a few months to build up sufficient endometrial nutrients and balance hormones. To be fair, we have also helped many people conceive during this 3-month time frame. But we really think doing the groundwork is best.
Preparing your body for conception truly makes a difference! Our experience is that patients who do this have easier pregnancies with fewer complications – these are the people with that gorgeous “pregnancy glow” who just feel great.
What happens during a session?
During the initial visit we discuss your medical and fertility history, menstrual history, and perform a physical examination. The physical examination consists of checking your pulse on your wrists, looking at the tongue, and diagnostic palpations, which gently checks specific reflex zones on the abdomen, neck, hands, and feet. The palpation offers further insights into the exact nature of the condition.
The resulting treatment plan may consist of acupuncture, custom tailored herbal medicine, nutritional supplements, daily basal body temperature charting according to the Fertility Awareness Method (Ehling/Singer, 2001), dietary adjustments, a movement plan, and stress reduction techniques.
LGBTQIA fertility
We believe that all people should have access to fertility treatments irrespective of marital status, sexual orientation, or gender. We love working with members of our queer community. Meridian Health Solutions strives to be an accessible resource and advocate for our patients as they go through ART processes such as IVF and IUI. Every person’s fertility journey is unique, important, and valid. We are honored to see each whole person and walk with them on the journey.
References
- Alternative medicine addresses many underlying causes of infertility, Feng J, Wang J, Zhang Y, Zhang Y, Jia L, Zhang D, Zhang J, Han Y, Luo S. The Efficacy of Complementary and Alternative Medicine in the Treatment of Female Infertility. Evid Based Complement Alternat Med. 2021 Apr 23;2021:6634309. doi: 10.1155/2021/6634309. PMID: 33986820; PMCID: PMC8093064.
- Acupuncture great for male and female infertility, Zhu J, Arsovska B, Kozovska K. Acupuncture Treatment for Fertility. Open Access Maced J Med Sci. 2018 Sep 19;6(9):1685-1687. doi: 10.3889/oamjms.2018.379. PMID: 30337989; PMCID: PMC6182526.
- Pomeranz B. Acupuncture Analgesia-Basic Research, Stux G, Hammershlag R (eds), Clinical Acupuncture: Scientific Basis, Berlin:Springer-Verlag, 2001. pp. 1-29
- Stener-Victorin E. Reduction of blood flow impedance in the uterine arteries of infertility women with electro-acupuncture. Human Reproduction, Vol.11, No.6, 1996. -- This study looked at women who had previously been diagnosed with a thin endometrial lining as a possible cause of fertility. The treatment group was given acupuncture for one month leading up to their IVF cycle and the uterine artery blood flow increased significantly within this time frame. This led to thicker endometrial lining in the treatment group versus the non-treatment group.
- Gerhard I. Gynecol Endocrinol. 1992;6(3):171-181. Infertility: Similar results to hormonal treatment but with fewer side effects.
- Emmons SL, Patton P. Acupuncture Treatment for infertile women undergoing intracytoplasmic sperm injection. Medical Acupuncture, A Journal for Physicians by Physicians, 2001 Vol. 12, No.2. – This study describes the use of acupuncture to stimulate follicle development in women undergoing in vitro fertilization. The case series included 6 women receiving intracytoplasmic sperm injection and acupuncture along with agents for ovarian stimulation. The results revealed no pregnancies occurred in the non-acupuncture cycles. Three women produced more follicles with acupuncture treatment (mean, 11.3 vs 3.9 prior to acupuncture; P=.005). All 3 women conceived, but only 1 pregnancy lasted past the 1st trimester. Acupuncture may be a useful adjunct to gonadotropin therapy to produce follicles in women undergoing in vitro fertilization. This study examined whether acupuncture stimulated follicle development in women undergoing IVF. The patients in the study had previously exhibited poor follicle development despite the use of gonadotropins. Acupuncture was used twice a week for 4 weeks leading up to egg retrieval the results showed that the non-treatment group had an average amount of 3.7 follicles whereas the acupuncture treatment group had an average of 8.4 follicles.
- Stener-Victorin E. Acta Obstet Gynecol Scand. 2000;79(3):180-8. Anovulation in PCOS: Electro-acupuncture appears to be useful to help stimulate ovulation in women with PCOS.
- Chang R, et al. Role of acupuncture in the treatment of female infertility. Fertility and Sterility, Dec 2002;78(6): -- Literature review of existing scientific rationale and clinical data for acupuncture for female infertility. Findings included positive effects on the central nervous system, influences on gonatropin secretion, and effects on uterine blood flow which affects endometrial thickness and morphology all of which are relevant for implantation. Acupuncture showed also significant improvements on stress related to infertility.
- Paulus W, et al. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertility and Sterility, April 2002;77(4):721-4. -- This study found that in a group of 160 women 80 who were treated with acupuncture before and after the embryo transfer phase of IVF had a 42.5% pregnancy rate vs. a 26.3% pregnancy rate in the non-treatment group.
- Zheng CH et al. Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization: a systematic review and meta-analysis. Fertility and Sterility, 2012 [Epub] – This is a meta-analysis of 24 randomized clinical trials for acupuncture and IVF, involving 5,807 participants. Clinical pregnancy rates and live birth rates were significantly higher in acupuncture groups as compared to sham or control groups.
- Westergaard LG, Mao Q, Krogslun M, Sandrini S, Lenz S, Grinsted J. Acupuncture on the day of embryo transfer significantly improves the reproductive outcome in infertile women: a prospective, randomized trial. Fertil Steril, 2006 May;85(5):1341-6. – This study was a repeat of the Paulus study above showing 39% higher rates of pregnancy in the acupuncture treatment group.
- Smith C, Coyle M, Norman RJ. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertil Steril, 2006 May;85(5):1352-8. -- In this single-blinded, randomized controlled trial using an acupuncture treatment group and a sham acupuncture group, the pregnancy rate was 31% in the acupuncture group vs. 23% in the control group. The ongoing pregnancy rate was higher in the treatment group: 28% vs. 18%.
- Magarelli PC, Cridennda DK, Cohen M. Changes in serum cortisol and prolactin associated with acupuncture during controlled ovarian hyperstimulation in women undergoing in vitro fertilization-embryo transfer treatment. Fertil Steril 2009 Dec;92(6):1870-9.
- Sinclair S. Male Infertility: Nutritional and environmental considerations. Altern Med Rev. 2000 Feb;5(1):28-38.
- Siterman S, Eltes F, Wolfson V, Lederman H, Bartoov B. Does Acupuncture treatment affect sperm density in males with very low sperm counts? A pilot study. Andrologia. 2000, Jan;32(1):31-9. The treatment group showed a significant improvement in sperm counts when compared to the control group which did not receive treatment.
- Fischl F, Riegler R, Bieglmayer C, Nasr F, Neumark J. Modification of semen quality by acupuncture in subfertile males. Geburtshilfe Frauenheilkunde, 1984 Aug;4498):510-2. – This study also looked at sperm counts and overall motility and morphology and found that the acupuncture treatment group showed significant higher counts when compared to the non-treatment group.
- Pei J, Strehler E, Noss U, et al. Quantitative evaluation of spermatozoa ultrastructure after acupuncture treatment for idiopathic male infertility. Fertility and Sterility July 2005;84(1):141-7.
- Ehling D, Singer K. Gauging a Woman’s Health by her Fertility Signals: Integrating Western with Traditional Chinese Medical Observations. Altern Ther Health Med. 1999;5(6):70-83. An analysis of using Fertility Awareness Method in conjunction with Oriental Medicine. Full article on www.orientalhealthsolutions.com/resources
- Soni S, Badawy SZ. Celiac disease and its effect on human reproduction: a Review: J Reprod Med. 2010 Jan-Feb;55(1-2):3-8
- Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Jolles M, Pinotti R, Swan SH. Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Hum Reprod Update. 2023 Mar 1;29(2):157-176. doi: 10.1093/humupd/dmac035. PMID: 36377604.

Diabetes & Blood Sugar Disorders
As of 2019, the CDC estimated over 37 million people in the U.S. (more than 11%) to have diabetes, and 1 in 3 adults have prediabetes. The USDA recommendations for a “healthy” diet, in the form of its previous Food Pyramid and now the Food Plate, are based on bad interpretations of science and nutrition. These guidelines have lead most of the U.S. and subsequently, the world, down a road of obesity and chronic disease, with diabetes spearheading the way.
Diabetes is a disease characterized by high levels of glucose in the blood. Glucose, the main energy source for cells in the body, is transported from the blood into cells by a hormone called insulin. Type I diabetes is an autoimmune condition involving destruction of the body’s insulin-producing cells. Type II diabetes, which makes up 95% of all diabetes cases, occurs when the body becomes resistant to insulin. The pancreas may also eventually stop producing sufficient amounts of insulin; both insulin resistance and insulin insufficiency lead to high blood glucose levels.
In both diabetes types I and II, glucose cannot enter cells, the body operates as if it were starved, and exhibits symptoms such as extreme thirst and hunger (especially craving sweets), fatigue, and frequent infections. Advanced stages of diabetes can result in kidney failure, tissue necrosis leading to amputations, and blindness.
Reactive Hypoglycemia
Reactive Hypoglycemia is defined as low levels of blood glucose. Symptoms include dizziness, shakiness, confusion, and when severe, coma or seizures. Mild hypoglycemia symptoms are quite common, and can occur when one skips meals or doesn’t consume enough protein and/or fat. Hypoglycemic episodes activate the adrenal glands’ cortisol output and trigger a physiological stress response.
Insulin Resistance
Insulin resistance refers to a state in which insulin receptor sites become less responsive, or “resistant,” to insulin, which is a hormone that lowers glucose in the blood.
Clinical Management
On a disease spectrum, reactive hypoglycemia usually manifests first, followed by mild to severe insulin resistance, and finally to full-blown diabetes. Both reactive hypoglycemia and insulin resistance have specific associated symptoms and blood test markers.
Recognizing the disorders early on, then applying appropriate nutritional management, is key in preventing diabetes and all the complications thereof. If diabetes has already been diagnosed, we focus on managing the secondary conditions associated with the disease using the methods below. 
Acupuncture to regulate the immune system, promote healthy circulation patterns, decrease the stress response, alleviate pain, and balance blood sugar metabolism;
Dietary counseling to target your unique constitution, and a nutrient-dense dietary program, based on scientific research, that has been shown to reverse diabetes.
Herbal and nutritional supplementation to improve your fundamental biological processes such as blood sugar regulation, hormonal balance, and immune and organ system function.
Lifestyle and movement recommendations help optimize each person's overall function, including blood sugar regulation.
Relevant studies:
Robeva R, Kirilov G, Tomova A, Kimanov P. Melatonin-Insulin Interactions in Patients with Metabolic Syndrome: J. Pineal Res. 2008 Jan;44(1):52-6
Davis SN, Tate D. Effects of morning hypoglycemia on neuroendocrine and metabolic responses to subsequent afternoon hypoglycemia in mornal men. J Clin Endocrinol Metab 2011 May;86(5):2043-50.
Davis SN et al. Effects of differing antecedent hypoglycemia on subsequent counterregulation in normal humans. Diabetes 1997 Aug;46(8):1328-35.
Burge et al. Effect of short-term glucose control on glycemic thresholds for epinephrine and hypoglycemic symptoms. J Clin Endocrinol Metab 2001 Nov;86(11):5471-8.
Scott, Scandart. Nocturnal cortisol release during hypoglycemia in diabetes. Diabetes Care 1981 Sept-Oct;4(5):514-8.
McGregor et al. Elevated endogenous cortisol reduces autonomoic neuroendocrine and symptom response at subsequent hypoglycemia. Am J Physiol Endocrinol Metab 2022 Apr;282(4):E770-7.
Davis et al. Role of cortisol in pathogenesis of deficient counterregulation after antecedent hypoglycemia in normal humans. J Clin Invest 1997 Jul 15;100(2):429-38.
Widdowson PS, et al. Inhibition of food response to intracerebroventricular injection of leptin is attenuated in rats with diet-induced obesity. Diabetes. 1997;46:1782-85.
Bosi E, et al. Increased intestinal permeability precedes clinical onset of type 1 diabetes: Diabetologia. 2006 Dec;49(12):2824-7. Epub 2006 Oct 7

Digestive Disorders
Digestive disorders are common afflictions that, according to a 2009 NIH study, affects 60-70 million Americans (1). In 2020, American made more than 8 million ER visits with digestive system diseases as the primary diagnosis (2). These numbers have been climbing as Americans’ dietary habits and food supply have deteriorated over the last few decades. The most common digestive disorders include constipation, diarrhea (including conditions like IBS, IBD, and SIBO), gallstones, acid reflux, hernia, gastritis, and hemorrhoids. Traditional East Asian medicine has also been shown to help immune conditions like Crohn's disease, celiac disease, and colitis.
Traditional East Asian Medicine’s View on the Digestive System
The digestive system is universally understood as a key player in extracting nutrients and energy from food and drink. In Traditional East Asian medicine, the two main organs involved with digestion are the Spleen and the Stomach, which receive and process food into qi and Blood that nourishes our bodies and minds. It should be noted that the Chinese Medicine understanding of the Spleen also includes the functions of the pancreas. If there is an imbalance in the Spleen or Stomach, then a variety of associated problems—ranging from pain, to chronic fatigue, to insomnia—can arise.
Traditional East Asian medicine has successfully treated digestive disorders for thousands of years. Treatise on Spleen and Stomach, written in the 13th century by the scholar and physician Li Gao, was the first known text to emphasize the centrality of a healthy digestive system, and the ideas found therein are still frequently used in contemporary practice.
Traditional East Asian Medicine Treatment Strategies
 One of Traditional East Asian medicine’s foundational principles emphasizes that every individual is unique. Even if two people present with similar complaints, the cause of illness for one person almost certainly differs from that of the other. Therefore every person’s course of treatment must be individually-tailored to suit his/her particular needs. Digestive disorders usually respond best to a combination of three types of therapies:
One of Traditional East Asian medicine’s foundational principles emphasizes that every individual is unique. Even if two people present with similar complaints, the cause of illness for one person almost certainly differs from that of the other. Therefore every person’s course of treatment must be individually-tailored to suit his/her particular needs. Digestive disorders usually respond best to a combination of three types of therapies:
Acupuncture is the insertion of sterile, thin needles into specific sites on the body. Selecting appropriate acupuncture points regulates proper qi or energy flow, which encourages one’s body to bring itself back into balance. When treating digestive disorders, acupuncture can help strengthen the Spleen and Stomach, regulate metabolism, and is especially useful in curbing GI-related acute pain.
Chinese Herbal Medicine (CHM) is a science and art supported by at least 2,000 years of empirical practice. Practitioners have always prescribed herbs to aid in digestion, promote nutrient absorption, and adjust appetites.
Nutrition is an essential component of good general health, and it is an especially important aspect for those with digestive disorders. Understanding a person’s dietary habits and nutritional needs provides the framework for implementing specific, effective dietary changes. The suggested changes usually involve introducing nutritious and delicious foods into the diet rather than depriving one of particular cravings. Often, simple dietary changes make a profound difference within one week.
*Increasingly, we are finding our patients to have food allergies and intolerances that affect their digestion and overall health. Learn more about food allergies/intolerances.
Western Medicine’s Approach
The Western Medicine treatment of digestive disorders frequently employs medications such as antacids, proton pump inhibitors, antibiotics, and steroids, which often carry undesirable side effects. For example, the Harvard Medical School Family Health Guide advises that proton pump inhibitors decrease the user’s stomach acid levels, which could lead to increased susceptibility to bacterial infections in the colon, pneumonia, and long-term use interferes with calcium and vitamin B12 absorption (3).
What Does the Research Say?
A large body of work is building up around the topic of Traditional East Asian Medicine and digestive disorders. One of the studies that gained wide recognition early on was a 1998 article that appeared in the Journal of the American Medical Association. In this randomized, double-blind, placebo-controlled trial concerning irritable bowel syndrome (IBS), it was found that both standardized and individually-tailored Chinese herbal formulas significantly improved the bowel symptoms and global quality of life experienced by IBS sufferers in the short term. However, at the 14-week follow-up, only those subjects who took the individually-tailored herbal formulas had sustained improvement (4).
An aspect of acupuncture that makes it so versatile is its ability to have a homeostatic effect on the body. For example, whether one has an overactive or underactive digestive system (i.e. diarrhea vs. constipation), acupuncture can help to regulate the disorder, and bring the system back into balance. This effect was studied by Xu, et al. In 2006, who found that the stimulation of acupuncture points traditionally used to treat digestive symptoms accelerated gastric emptying in patients with delayed bowel responses, and relieved dyspepsia in subjects with normal gastric emptying (5).
One of the most promising fields for the use of acupuncture is in the field of functional gastric disorders. “Functional disorder” refers to any condition in which the function, or normal operation, of the body is disrupted, but at the same time, exams show no identifiable anatomical or structural abnormalities. In these cases, Western medicine has much difficulty finding the appropriate treatment modalities.
Because Traditional East Asian medicine views the person as a whole, the treatment approach of a “functional disorder” is no different from other disorders. Clinical research is recognizing that acupuncture may be useful in functional disorders “because it has been shown to alter acid secretion, GI motility, and visceral pain” (6). As such, acupuncture is showing promise in the treatment of gastroesophageal reflux disease (GERD), functional dyspepsia (FD), irritable bowel syndrome (IBS), postoperative nausea/vomiting, and even visceral hypersensitivity (6).
References
1. National Institutes of Health, U.S. Department of Health and Human Services. Opportunities and Challenges in Digestive Diseases Research: Recommendations of the National Commission on Digestive Diseases. Bethesda, MD: National Institutes of Health; 2009. NIH Publication 08–6514.
2. National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2020 Emergency Department Summary Tables
3. Bensoussan et al. Treatment of irritable bowel syndrome with Chinese herbal medicine: a randomized controlled trial. JAMA. 1998 Nov 11;280(18):1585-9.
4. Xu, et al. Electroacupuncture accelerates solid gastric emptying and improves dyspeptic symptoms in patients with functional dyspepsia. Dig Dis Sci. 2006 Dec;51(12):2154-9.
5. Takahashi, T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol. 2006 May;41(5):408-17.
Other relevant studies:
Ohman L, Simren M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions: Nat Rev Gastroenterol Hepatol. 2010 Mar:7(3):163-73. Epub 2010 Jan 26
Lydiard RB. Irritable bowel syndrome, anxiety, and depression: What are the links? J Clin Psychiatry. 2001;62 Suppl 8:38-45; discussion 46-7
O’Mahony SM, et al. Early life stress alters behavior, immunity, and microbiota in rats: implications for Irritable Bowel Syndrome and psychiatric illnesses: Biol Psychiatry. 2009 Feb 1;65(3):263-7. Epub 2008 Aug 23
Kwan CL, et al. Abnormal forebrain activity in functional bowel disorder patients with chronic pain: Neurology 2005 Oct 25;65(8):1268-77
Tache Y, et al. Brain regulation of gastric acid secretion by neurogastrointestinal peptides: Peptides. 1981;suppl 2:51-5
Savidge TC, et al. Enteric glia regulate intestinal barrier function and inflammation via release of S-nitrosoglutathione: Gastroenterology. 2007 Apr;132(4):1344-58. Epub 2007 Feb 1
Geissler A, et al. Focal white-matter lesions in patients with inflammatory bowel disease: Lancet 345: 897-898;1995
Wade PR, Cowen T. Neurodegeneration: a key factor in the ageing gut: Neurogastroenterol Motil. 2004 Apr;16 Suppl 1:19-23
Photo © Dagmar Ehling

Brain & Memory
Is your memory not what it used to be? Do you have difficulty focusing on your work? Do you have trouble remembering people’s names? Do you experience anxiety that seems out of proportion compared to the stress in your life?
Brain function encompasses many areas, including memory, focus, space-time orientation, the ability to learn new skills, and mental-emotional states. Recent public health figures show alarming increases in brain function disorders for people of all ages:
the Alzheimer's Association data from 2022 show that 1 in 9 Americans over age 65 have Alzheimer's dementia. The CDC reports that 9.5% of American children ages 4-17 have been diagnosed with ADHD; over 10% adults suffer from depression and nearly 40 million adult Americans (or 18%) suffer from anxiety disorders. For anxiety disorders alone more than $22.84 billion is spent annually for repeated use of health care services.
Many neurological and brain disorders are not yet well-understood. Causative factors include neurodegeneration (death of brain cells), viral infections, environmental toxins, and genetic predisposition. Depending on the condition, conventional Western medicine treatment may include a multitude of medications, surgery, or behavioral therapy.
The practitioners at MHS understand brain health to be a direct extension of health in the rest of the body. Many factors, such as blood sugar disregulation, poor oxygenation to the brain, food intolerances, poor digestive health leading to leaky gut/leaky blood-brain -barrier, systemic inflammation, and adrenal hyper/hypofunction could contribute to a decline in brain health. We are trained to recognize signs associated with imbalances in specific neurotransmitters, and address most cases with these treatment approaches: 
Acupuncture protocols that specifically address brain injury, regulate feedback between the peripheral and central nervous systems, promote healthy circulation patterns, and modulate the stress response. Acupuncture has long been used as a treatment to help improve memory and cognitive function. A 2006 study in Neurology Research demonstrated that acupuncture significantly helped with test subjects’ memory and calculation1. Recent clinical studies are also showing that acupuncture helps with anxiety, depression, and control insomnia2, and even improve the immune response of people with anxiety3.
Dietary counseling to target your unique constitution, decrease inflammation, and provide optimal nutrition for brain health;
Herbal and nutritional supplementation that helps to balance oxygen and glucose levels in the body, and positively impact central nervous system function.
Lifestyle practices such as appropriate exercise, sleep regulation, stress and mental health management all play a role in brain health.
With a combination of the above approaches, we have successfully helped many people with the following:
- Dramatically improve spacial and verbal memory
- Enhance focus and work performance
- Manage anxiety associated with PTSD
- Regulate moods
- Decrease anxiety & depression
- Working in conjunction with the patient’s physician, manage a decrease and/or discontinuation of antidepressant medications
- Help children with impulse control, tics, and sensory disintegration disorder
- Improve ADHD behaviors in children and adults
References:
1. Yu et al., Effect of acupuncture treatment on vascular dementia. Neurol Res. 2006 Jan;28(1):97-103.
2. Ruan et al., Effects of the degrees of anxiety and depression on the therapeutic effect of acupuncture in the patient of insomnia. Zhongguo Zhen Jiu. 2006 Mar;26(3):186-8.
3. Arranz, et al. Effect of acupuncture treatment on the immune function impairment found in anxious women. Am J Chin Med. 2007;35(1):35-51.
Other relevant Studies:
Luo H, Meng F, Jia Y, Zhao X: Clinical research on the therapeutic effect of the electro-acupuncture treatment in patients with depression. Psychiatry and Clinical Neurosciences 1998; 52 (Suppl):S338-S340.
Ernst E, Rand Jl, Stevinson C: Complementary therapies for depression: an overview. Archives of General Psychiatry 1998; 55:1026-1032.
Kurland HD. ECT and Acu-EST in the treatment of depression. American Journal of Chinese Medicine 1976; 4:289-292.
Roschke J, Wolf C, Kogel P, Wagner P, Bech S: Adjuvant whole body acupuncture in depression. A placebo-controlled study with standardized mianserin therapy. [German] Nervenarzt 1998; 69:961-967.
Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions: Nat Rev Gastroenterol Hepatol. 2010 Mar:7(3):163-73. Epub 2010 Jan 26
Wade PR, Cowen T. Neurodegeneration: a key factor in the ageing gut: Neurogastroenterol Motil. 2004 Apr;16 Suppl 1:19-23
Maes M, Kubera M, Leunis JC. The brain-gut barrier in major depression: Intestinal mucosal dysfunction with an increased translocation of LPS from gram negative interobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression: Neuro Endocrinol Lett. 2008 Feb;29(1):117-24
Reichelt KL, Knivsberg AM. The possibility and probability of a gut-to-brain connection in autism: Ann Clin Psychiatry. 2009 Oct-Dec;21(4):205-11

Infertility
The superior physician does not just treat disease but teaches society and helps form the intentions of humanity. ~Sun Si Miao 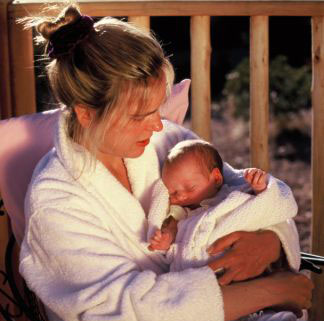
The Western View:
Definition: After one year of unprotected intercourse without having achieved pregnancy a couple is considered infertile. If a medical cause for infertility is discovered, various treatment options can be entertained including Traditional Asian medicine. 10% of American couples suffer from infertility. Among infertile couples, about 40% are due to female infertility, 40% are due to male infertility, 10% have both female and male factor whereas 10% have unexplained causes. Unexplained Infertility: While the causes are unknown, these couples are still encouraged to try treatment. Couples with unexplained infertility often find acupuncture and Oriental medicine to be a non-invasive, inexpensive way to offer a new perspective on their fertility process. Female Infertility: Ovulation disorders, fallopian tube obstruction and scarring, uterine and cervical disorders, endometriosis, immunological factors, polycystic ovaries, (premature) ovarian failure. Male Infertility: Low sperm count, abnormal sperm morphology, poor motility, varicocele, immunological factors, ejaculation disorders. Western Medical Treatment Options: Ovulation induction through gonadotropin injections, artificial insemination (IUI) with or without the use of gonadotropins, In- Vitro Fertilization (IVF), Gamete Intrafallopian Transfer (GIFT), Zygote Intrafallopian Transfer (ZIFT), Intracytoplasmic Sperm Injection (ICSI), Epididymal and testicular sperm extraction, freezing of sperm and embryos, donor eggs, sperm or embryos, surrogate parenting, and adoption. Acupuncture has been a recent addition to many ART clinic programs in Europe and the United States. How can I enhance my fertility? Traditional Asian Medicine (TAM) has long been known to treat both female and male infertility. Infertility seems to be on the rise though it appears mostly to be related to the fact that today’s couples delay child-bearing. Infertility affects about one in six couples. Anovulation, amenorrhea, short luteal phase, or various hormonal imbalances may be the cause though there are many other reasons why infertility persists. TAM teaches that fertility is a woman’s natural state between the onset of her menstruation and menopause. Problems with fertility in both men and women result from imbalances within the organ systems, hormones, and energy networks or acupuncture meridians. The premise for Traditional Asian Medicine in the treatment of infertility is to create a hospitable environment in a woman’s womb. This can be achieved using herbs, acupuncture, and nutrition. In traditional cultures, couples typically prepared themselves six months prior to conception by eating specific nutrient-dense, fertility-enhancing foods. Eating these types of foods which are based on an Oriental medical diagnosis can positively influence a couple’s ability to conceive. Couples coming to Oriental Health Solutions will receive a detailed meal plan.
What can Traditional Asian Medicine and Acupuncture do for my partner’s and my infertility problem?
 Traditional Asian medicine offers a natural, non-invasive approach to treating infertility by focusing on enhancing the quality of eggs, sperm, endometrial lining and cervical fluid. Sometimes this approach is sufficient for couples to conceive on their own and it offers a valuable adjunct for couples who are about to undergo the expense and physical demands of IVF. Acupuncture may also support patients during in vitro fertilization, artificial insemination, and gonadotropin assisted cycles using your own eggs or those of a donor. Studies have shown that acupuncture increases the success rate of ART and helps to alleviate side-effects (Paulus et al, 2001). Acupuncture is a low-cost, noninvasive, safe treatment, and has virtually no side effects. It’s a great adjunct treatment to western medical procedures. A CBS News article in 2004 described the merits of using acupuncture for the treatment of infertility in which it described how couples are turning more frequently to acupuncture to enhance their fertility and in vitro fertilization outcomes and the importance of finding a qualified and experienced practitioner to treat underlying problems (CBS news 2004). A study published in Fertility & Sterility (Diane Cridennda LAc and Paul Magarelli MD, 2009) were able to show how acupuncture enhances IVF outcomes as well as explain methods of action. Click on the photo above to listen to a Dawn Davenport's radio interview on the subject.
Traditional Asian medicine offers a natural, non-invasive approach to treating infertility by focusing on enhancing the quality of eggs, sperm, endometrial lining and cervical fluid. Sometimes this approach is sufficient for couples to conceive on their own and it offers a valuable adjunct for couples who are about to undergo the expense and physical demands of IVF. Acupuncture may also support patients during in vitro fertilization, artificial insemination, and gonadotropin assisted cycles using your own eggs or those of a donor. Studies have shown that acupuncture increases the success rate of ART and helps to alleviate side-effects (Paulus et al, 2001). Acupuncture is a low-cost, noninvasive, safe treatment, and has virtually no side effects. It’s a great adjunct treatment to western medical procedures. A CBS News article in 2004 described the merits of using acupuncture for the treatment of infertility in which it described how couples are turning more frequently to acupuncture to enhance their fertility and in vitro fertilization outcomes and the importance of finding a qualified and experienced practitioner to treat underlying problems (CBS news 2004). A study published in Fertility & Sterility (Diane Cridennda LAc and Paul Magarelli MD, 2009) were able to show how acupuncture enhances IVF outcomes as well as explain methods of action. Click on the photo above to listen to a Dawn Davenport's radio interview on the subject.
How does Traditional Asian Medicine and Acupuncture affect our fertility?
Researchers have examined that acupuncture points are conductors of electromagnetic impulses. Stimulating these points along their pathways via acupuncture enables the release of endorphins and stimulates immune system cells to specific sites. It activates opioids within the central nervous system, which is associated with pain reduction. Acupuncture has been shown to alter brain activity, body sensations and autonomic nervous system functions. Acupuncture impacts autonomic nervous system functions such as immune reactions, blood pressure, blood flow, and body temperature regulation. It alters brain chemistry by changing the release of neurotransmitters and neuro-hormones in a beneficial way. Studies show promising data that acupuncture may affect the menstrual cycle by changing neuroendocrine effects on the body. This means that different combinations of acupuncture points may play a role in the release of the hormones responsible for regulating a woman’s menstrual cycle and enhancing a couple’s fertility. (Pomeranz et al, 2001)
How does stress affect fertility?
Research has shown that acupuncture treatments reduce stress, a common occurrence for couples dealing with infertility. Stress alters the subtle balance between the hypothalamus, pituitary and reproductive organs which is why stress, among other factors, may contribute to irregular menstruation and/or premenstrual syndrome. A stressed woman is generally tense, and may, therefore, suffer more likely from spasms in the fallopian tubes and the uterus which may disrupt implantation. Stress also makes her susceptible to mood swings. Acupuncture releases endorphins thereby counters the negative effects of stress. Many patients experience acupuncture as a very relaxing experience that is likely related to the release of endorphins (Chang et al, 2002).
Can Acupuncture, diet and Chinese herbs help build a woman’s endometrial lining?
Acupuncture has been shown to increase blood flow to the reproductive organs. Healthy blood supported by a healthy, nutrient-dense diet will provide the ovaries and uterus with more nourishment. The Chinese pharmacopeia offers many blood tonics that enrich the endometrial lining. Increased blood flow improves follicle and egg health and promotes the lining of the uterus to create a hospitable environment for an embryo to implant and grow. This holds true whether the woman is undergoing gonadotropin therapy or is attempting to conceive naturally (Stener-Victorin, 1998).
How does Traditional Asian Medicine address my high FSH levels?
Women who have elevated FSH levels may benefit from increased blood flow to the reproductive organs and thereby create balance within the endocrine system. FSH levels can fluctuate and unfortunately, having one FSH test result is only a window into what is going on at that specific time. Traditional Asian medicine offers both acupuncture and Chinese herbal therapy to women who are in this situation and many times treatment is successful allowing her to conceive naturally or with the help for Assisted Reproductive Technology (ART). Specific herbs have been known for thousands of years to enhance the health of follicles.
How does acupuncture benefit conception?
Strengthening the immune system plays a very important role in conception. Acupuncture helps to adjust the amount of white blood cells, T-cells and antibodies in the body thereby regulating the body’s immune system. This is relevant when there are immunological reasons for infertility, failed implantation problems, or repeated miscarriages. Inflammation, so common in the general population, can also have an effect on the reproductive system. Women with endometriosis typically present with some type of systemic inflammation as well as circulatory problems. Acupuncture also fosters receptivity by opening the energy pathways (meridians). There are many benefits to using acupuncture, herbal therapy, targeted diets, and nutritional supplements to effectively curb the inflammatory response. (Gerhard 1992 ; Emmons et al, 2001)
I have had several miscarriages. How can Asian Medicine help?
Women who suffer from repeated miscarriages either have an imbalanced immune system, or undernourished reproductive system. A thorough health history and analysis will determine how this issue should be addressed. Often, women benefit greatly from eating a nutrient-dense diet, supplemention with omega-3 fatty acids and taking herbs for a short time to nourish the reproductive organs. Additionally, acupuncture treatments may assist pregnant women in preventing a miscarriage.
I was diagnosed with PCOS. What can you offer?
An estimated 10% of childbearing women have Polycystic Ovarian Disease (PCOS). PCOS is a disorder that typically presents with obesity, hirsutism (unusual hair growth in the face, chest, abdomen, etc), and acne. An ultrasound reveals many unripe fluid-filled sacs around the ovaries. Many women suffer from anovulation and subsequent amenorrhea (no periods) and some have regular or irregular cycles. Many women have high levels of male hormones, also known as androgens. In women with PCOS, the ovaries do not produce all the hormones they need for follicles to fully mature. The follicles start to grow, but merely become cysts rather than fully-developed eggs. Because mature eggs secrete progesterone, progesterone is not produced in PCOS patients. Instead, the cysts may produce male hormones, which in turn prevent ovulation. Some of these women have insulin resistance and are prone to type-2 diabetes, high cholesterol, high blood pressure, patches of thickened skin and dark brown or black skin on the neck, arms, breasts, or thighs. The exact cause of PCOS is unclear, but it is hypothesized that PCOS is linked to insulin-resistance. Therefore, maintaining a healthy diet that is devoid of sugar, starches and simple carbohydrates may be very important. Both acupuncture and herbal medicine can help to regulate insulin levels and balance the endocrine system. (Stener-Victorin, 2000)
Can Acupuncture enhance the outcome of Assisted Reproductive Therapy (ART)?
Couples who have good quality eggs, sperm, and endometrial lining typically have better outcomes when using ART. Many traditional cultures encouraged couples who were ready to conceive to eat sacred, nutrient-dense diets for about six months prior to trying to conceive. Oriental medicine also advocates the use of special fertility diets for couples who are attempting natural conception or use ART. ART has higher success rates if the the uterine terrain is abundant with nutrients, and the woman’s endocrine system is balanced. (Paulus et al, 2001; Chang et al, 2002; Westergaard et al, 2006; Smith et al, 2006)
What about the side-effects of ART?
Acupuncture may help to reduce the side effects some women experience from the medications and the stress of the IVF experience. With acupuncture’s calming and balance-enhancing effects, women tend to feel more relaxed and centered. Acupuncture helps treat abdominal bloating, mood swings, hot flashes and headaches that women may experience during the ART cycle.
How can Traditional Asian Medicine help sperm count, morphology and motility?
In men, infertility may be due to a systemic issue or a life-style problem. Male sperm counts in the U.S. have diminished by 50% since 1945 (Sinclair 2000). This may be due to dietary changes, xeno-estrogens (estrogen-like components in pesticides and herbicides in the environment), heavy metals and other environmental factors. An estimated 10% of men are infertile, and the male partner is a factor in up to 50% of infertile couples. In many cases, the exact cause of male infertility is unknown. Several studies indicate that acupuncture treatments may significantly improve total functional sperm, the percentage of sperm viability, and the total motile spermatozoa per ejaculate. These results were obtained by taking sperm samples from the men before and after one to three months of acupuncture treatment. (Siterman et al, 2000; Fischl et al, 1984 ) Pei et al, found that acupuncture improved sperm production and motility (a measure of forward movement of sperm). Sperm samples were analyzed at the beginning and end of the study and showed significant improvements in sperm quality in the acupuncture group compared with the other group. Acupuncture treatment showed fewer structural defects in the sperm and an increase in the number of normal sperm in ejaculate. But other sperm abnormalities, such as immature sperm or sperm death, remained unchanged by acupuncture. The researchers state that acupuncture treatment is a simple, noninvasive method that can improve sperm quality. (Pei et al, 2005)
How many treatments will I need?
Many couples experience a sense of urgency as their biological clock is ticking. It is, however, important to remember that conception is a process of “receiving”. Therefore, it is crucial that the couple stays as relaxed as possible. It is helpful to complete about three months of treatment using either acupuncture and/or Chinese herbs (depending on your specific circumstance) due to the time needed to balance your system. However, we have helped many patients to conceive during that time frame. Here at MHS, our practitioners have decades of experience, and are always happy to work with you and your doctor in order to best fit your needs.
Does every Acupuncturist have additional training for the Treatment of Infertility?
In 2006, the American Board of Oriental Reproductive Endocrinology ([url=http://www.aborm.org]http://www.aborm.org[/url]) was founded. Its goal is to provide certification for Oriental medical practitioners to ensure qualified knowledge, experience, and the ability to effectively interact with reproductive endocrinologists, as the treatment of infertility is currently not part of a standard Oriental medical school curriculum. Please view their website for a nationwide list of certified practitioners.
Assisted Reproductive Clinics Nationwide
http://www.sart.org/find_frm.html
Testimonials:
Happy New Year! I hope this card finds you well. I’ve meaning to mail this check for weeks now. I am sorry it’s so tardy. Our little boy is miraculously still in my belly. We’ve named him Tim for his strength and endurance. I hope you’re doing well and please know how much I appreciate all of your love and support throughout this pregnancy. Love, B. and F. B., Durham, NC Thank you so much!!! Without you we wouldn’t have had our little girl. After five years of trying to conceive… She is so precious and strong. I sailed through the pregnancy and our daughter is vital and so very beautiful. Thank you for your helping hand to bring her here! And thank you for the work you do! I can’t believe she is here. With gratitude, M.E. Chapel Hill It took four painful miscarriages until I came to see you. You patiently explained to me about specific foods, I drank those god-awful herb teas and in three months I was pregnant. I now hold my little girl in my arms and we still can’t believe it. After all these years of emotional roller coasters! Thank you so very much. God bless you! C.V. Chapel Hill I wanted to thank you again for all your wonderful support getting me prepared for pregnancy. I think it made a tremendous difference; I'll never know for certain, but I'd guess it would have been very difficult for me to now have a child without your efforts. If you are interested, here's a link to some additional pictures of our son. (I have to laugh that I didn't know that the picture of me below would also be destined to show up on the Kodak site's advertising blitz; just what everyone wants -- a mug with my belly on it!!) Anyway, thanks for all you do for me and so many others. Big hug and lots of admiration~ K.B., Durham, NC This was an email communication from a patient to her western medical physician: I thought you might like to see a picture of my daughter born recently. It is really too long of a story for email-- but my healing journey started with my appointments with you and your suggestions of seeing several other people. Over the past 2 years, I've received acupuncture off and on to build up my immune system and get rid of my chronic sinusitis and sore throat that I had for a year and a half. Even though I had another miscarriage in the fall of 04 the physical healing from that was much easier and I was able to recover from that physically and even emotionally better. But I would say if you asked me last January if I would have a baby this January, I would have been rather doubtful that it would happen. But then by some miracle I think we conceived on my husband's 40th birthday. This time I had my pregnancy monitored by the reproductive endocrinology group, got acupuncture and herbs for a few weeks early in the pregnancy for miscarriage prevention and had a healthy pregnancy. I also did the acupuncture program during the last 4 weeks of pregnancy to prepare my body for a smooth labor and had my pelvis aligned by my chiropractor and I prayed. A Lot! The practitioner at OHS is very good and I thank you for telling me about the clinic! My delivery on New Year's Eve couldn't have gone better-- I worked with a doula and had another totally natural childbirth (my third) after having a C-section in ‘97 with my first child. But this was the smoothest labor by far. This labor went fast-- I only had about 1 hr of tough contractions and then my daughter basically jumped out of me-- she popped her head and shoulders out before my doctor was even there. Her birth has brought so much healing to me and to my whole family and I feel incredibly grateful. Best wishes to you for the New Year! B. F., Chapel Hill, NC Here finally is a picture of our son. He is so strong and happy. Thank you for all your hard work and commitment to bring him here. I had no idea this would be possible with all those years of anovulation. It is a miracle! He is a miracle! God bless you!” H.V., Durham, NC  I just wanted to let you know how much I appreciate all of your assistance. Your kind manner and open ears really helped me to get my body in balance and accomplish my goals. I am now 13 weeks pregnant and feeling great. I had some problems with bleeding but after my most recent ultrasound my baby is fine. Thanks again for everything and I wish the best for you and all of your patients. I‘m sure I’ll see you in the future. God Bless, J. S., Roxboro, NC PS: I’ll keep you posted. I am due Christmas day! I hope all is well with you. I think about you often and I am so thankful for everything you did for my husband and I. Being a mother is so much more than I ever imagined. Our daughter is such a blessing. We are so fortunate to have her in our lives. She is doing very well. Growing, playing, laughing and making every moment so precious. She is growing so fast and looks like a little girl. My husband mentioned he stopped by to see you a few months ago when I was interviewing at Duke. I am so glad you were able to see our cutie. I did get the job and my work schedule is much more conducive to having a family than my previous job. Since I switched jobs, I have to switch doctors. I am so upset about having to leave my original doctor in Chapel Hill. They were absolutely wonderful throughout my whole pregnancy. Do you have a recommendation for a new OB/GYN that you work with that accepts my new insurance? I know not all doctors believe in alternative medicine and I want to make sure my new doctor does because I am confident that what you did for us resulted in our beautiful daughter. Thank you! M. E., Mebane, NC I hope your week is going well. I just wanted to touch base with you with some rather surprising development. When I saw you last week, I told you I was premenstrual. Well, those symptoms went away and this morning was my 18th day since ovulation with my temperature remaining very high. So I took a pregnancy test and it was positive! You can imagine my surprise after 3 ½ years of trying and 3 failed IVF cycles! My husband says you must have quite the magic touch!!! We’re obviously excited and rather stunned but we’re trying not to get carried away until we see what happens. I was just wondering whether you suggest I continue taking the herbs you gave me or should I stop? Thanks! L.B., Cary, NC Greetings from a former patient: You may recall that I came to see you for multiple (5) miscarriages and you successfully helped me get pregnant with twins, then carry them to term. My family moved out of state shortly after the twins were born. We were SHOCKED about a year later to find ourselves pregnant with our fourth child -- even more surprised that the pregnancy worked. You broke the miscarriage pattern, indeed! I still can't believe I went from unexplained infertility to mom of four. I hope you're doing well, and I continue to have very fond memories of you and your work helping to create our wonderful family. Best, A.F., Portland, ME
I just wanted to let you know how much I appreciate all of your assistance. Your kind manner and open ears really helped me to get my body in balance and accomplish my goals. I am now 13 weeks pregnant and feeling great. I had some problems with bleeding but after my most recent ultrasound my baby is fine. Thanks again for everything and I wish the best for you and all of your patients. I‘m sure I’ll see you in the future. God Bless, J. S., Roxboro, NC PS: I’ll keep you posted. I am due Christmas day! I hope all is well with you. I think about you often and I am so thankful for everything you did for my husband and I. Being a mother is so much more than I ever imagined. Our daughter is such a blessing. We are so fortunate to have her in our lives. She is doing very well. Growing, playing, laughing and making every moment so precious. She is growing so fast and looks like a little girl. My husband mentioned he stopped by to see you a few months ago when I was interviewing at Duke. I am so glad you were able to see our cutie. I did get the job and my work schedule is much more conducive to having a family than my previous job. Since I switched jobs, I have to switch doctors. I am so upset about having to leave my original doctor in Chapel Hill. They were absolutely wonderful throughout my whole pregnancy. Do you have a recommendation for a new OB/GYN that you work with that accepts my new insurance? I know not all doctors believe in alternative medicine and I want to make sure my new doctor does because I am confident that what you did for us resulted in our beautiful daughter. Thank you! M. E., Mebane, NC I hope your week is going well. I just wanted to touch base with you with some rather surprising development. When I saw you last week, I told you I was premenstrual. Well, those symptoms went away and this morning was my 18th day since ovulation with my temperature remaining very high. So I took a pregnancy test and it was positive! You can imagine my surprise after 3 ½ years of trying and 3 failed IVF cycles! My husband says you must have quite the magic touch!!! We’re obviously excited and rather stunned but we’re trying not to get carried away until we see what happens. I was just wondering whether you suggest I continue taking the herbs you gave me or should I stop? Thanks! L.B., Cary, NC Greetings from a former patient: You may recall that I came to see you for multiple (5) miscarriages and you successfully helped me get pregnant with twins, then carry them to term. My family moved out of state shortly after the twins were born. We were SHOCKED about a year later to find ourselves pregnant with our fourth child -- even more surprised that the pregnancy worked. You broke the miscarriage pattern, indeed! I still can't believe I went from unexplained infertility to mom of four. I hope you're doing well, and I continue to have very fond memories of you and your work helping to create our wonderful family. Best, A.F., Portland, ME
References
1. CBS News, New York, July 24, 2004. http://www.cbsnews.com/stories/2004/07/23/earlyshow/saturday/main631441.shtml
2. Pomeranz B. Acupuncture Analgesia-Basic Research, Stux G, Hammershlag R (eds), Clinical Acupuncture: Scientific Basis, Berlin:Springer-Verlag, 2001. pp. 1-29
3. Stener-Victorin E. Reduction of blood flow impedance in the uterine arteries of infertility women with electro-acupuncture. Human Reproduction, Vol.11, No.6, 1996. -- This study looked at women who had previously been diagnosed with a thin endometrial lining as a possible cause of fertility. The treatment group was given acupuncture for one month leading up to their IVF cycle and the uterine artery blood flow increased significantly within this time frame. This led to thicker endometrial lining in the treatment group versus the non-treatment group.
4. Gerhard I. Gynecol Endocrinol. 1992;6(3):171-181. Infertility: Similar results to hormonal treatment but with fewer side effects.
5. Emmons SL, Patton P. Acupuncture Treatment for infertile women undergoing intracytoplasmic sperm injection. Medical Acupuncture, A Journal for Physicians by Physicians, 2001 Vol. 12, No.2. – This study describes the use of acupuncture to stimulate follicle development in women undergoing in vitro fertilization. The case series included 6 women receiving intracytoplasmic sperm injection and acupuncture along with agents for ovarian stimulation. The results revealed no pregnancies occurred in the non-acupuncture cycles. Three women produced more follicles with acupuncture treatment (mean, 11.3 vs 3.9 prior to acupuncture; P=.005). All 3 women conceived, but only 1 pregnancy lasted past the 1st trimester. Acupuncture may be a useful adjunct to gonadotropin therapy to produce follicles in women undergoing in vitro fertilization. This study examined whether acupuncture stimulated follicle development in women undergoing IVF. The patients in the study had previously exhibited poor follicle development despite the use of gonadotropins. Acupuncture was used twice a week for 4 weeks leading up to egg retrieval the results showed that the non-treatment group had an average amount of 3.7 follicles whereas the acupuncture treatment group had an average of 8.4 follicles.
6. Stener-Victorin E. Acta Obstet Gynecol Scand. 2000;79(3):180-8. Anovulation in PCOS: Electro-acupuncture appears to be useful to help stimulate ovulation in women with PCOS.
7. Chang R, et al. Role of acupuncture in the treatment of female infertility. Fertility and Sterility, Dec 2002;78(6): -- Literature review of existing scientific rationale and clinical data for acupuncture for female infertility. Findings included positive effects on the central nervous system, influences on gonatropin secretion, and effects on uterine blood flow which affects endometrial thickness and morphology all of which are relevant for implantation. Acupuncture showed also significant improvements on stress related to infertility.
8. Paulus W, et al. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertility and Sterility, April 2002;77(4):721-4. -- This study found that in a group of 160 women 80 who were treated with acupuncture before and after the embryo transfer phase of IVF had a 42.5% pregnancy rate vs. a 26.3% pregnancy rate in the non-treatment group.
9. Westergaard LG, Mao Q, Krogslun M, Sandrini S, Lenz S, Grinsted J. Acupuncture on the day of embryo transfer significantly improves the reproductive outcome in infertile women: a prospective, randomized trial. Fertil Steril, 2006 May;85(5):1341-6. – This study was a repeat of the Paulus study above showing 39% higher rates of pregnancy in the acupuncture treatment group.
10. Smith C, Coyle M, Norman RJ. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertil Steril, 2006 May;85(5):1352-8. -- In this single-blinded, randomized controlled trial using an acupuncture treatment group and a sham acupuncture group, the pregnancy rate was 31% in the acupuncture group vs. 23% in the control group. The ongoing pregnancy rate was higher in the treatment group: 28% vs. 18%.
11. Sinclair S. Male Infertility: Nutritional and environmental considerations. Altern Med Rev. 2000 Feb;5(1):28-38.
12. Siterman S, Eltes F, Wolfson V, Lederman H, Bartoov B. Does Acupuncture treatment affect sperm density in males with very low sperm counts? A pilot study. Andrologia. 2000, Jan;32(1):31-9. The treatment group showed a significant improvement in sperm counts when compared to the control group which did not receive treatment.
13. Fischl F, Riegler R, Bieglmayer C, Nasr F, Neumark J. Modification of semen quality by acupuncture in subfertile males. Geburtshilfe Frauenheilkunde, 1984 Aug;4498):510-2. – This study also looked at sperm counts and overall motility and morphology and found that the acupuncture treatment group showed significant higher counts when compared to the non-treatment group.
14. Pei J, Strehler E, Noss U, et al. Quantitative evaluation of spermatozoa ultrastructure after acupuncture treatment for idiopathic male infertility. Fertility and Sterility July 2005;84(1):141-7.
15. Ehling D, Singer K. Gauging a Woman’s Health by her Fertility Signals: Integrating Western with Traditional Chinese Medical Observations. Altern Ther Health Med. 1999;5(6):70-83. An analysis of using Fertility Awareness Method in conjunction with Oriental Medicine. Full article on [url=http://www.orientalhealthsolutions.com/resources]http://www.orientalhealthsolutions.com/resources[/url]
16. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83

Digestive Disorders
Overview
Digestive disorders are common afflictions that, according to the National Health Interview Survey done in 1996, affected 60-70 million Americans(1). There were over 230,000 deaths, including cancer cases. These numbers have only increased as Americans’ dietary habits and food supply have deteriorated over the last decade. The most common digestive disorders include abdominal wall hernia, Liver disorders such as hepatitis and cirrhosis, constipation, gallstones, reflux, gastritis, inflammatory bowel disease, irritable bowel syndrome, diarrhea, and hemorrhoids.
Oriental Medicine’s View on the Digestive System
 The digestive system is universally understood as a key player in extracting nutrients and energy from food and drink. In Oriental medicine, the two main organs involved with digestion are the Spleen and the Stomach, which are said to receive, and then process food into Qi and Blood that nourishes our bodies and minds. It should be noted that the ancient Chinese understanding of the Spleen also includes the functions of the pancreas. If there is an imbalance in the Spleen or Stomach, then a huge variety of associated problems—ranging from pain, to chronic fatigue, to insomnia—can arise. Oriental medicine has successfully treated digestive disorders for thousands of years. Treatise on Spleen and Stomach, written in the 13th century, was the first known text to emphasize the centrality of a healthy digestive system, and the ideas found therein are still frequently used in contemporary practice.
The digestive system is universally understood as a key player in extracting nutrients and energy from food and drink. In Oriental medicine, the two main organs involved with digestion are the Spleen and the Stomach, which are said to receive, and then process food into Qi and Blood that nourishes our bodies and minds. It should be noted that the ancient Chinese understanding of the Spleen also includes the functions of the pancreas. If there is an imbalance in the Spleen or Stomach, then a huge variety of associated problems—ranging from pain, to chronic fatigue, to insomnia—can arise. Oriental medicine has successfully treated digestive disorders for thousands of years. Treatise on Spleen and Stomach, written in the 13th century, was the first known text to emphasize the centrality of a healthy digestive system, and the ideas found therein are still frequently used in contemporary practice.
Oriental Medicine Treatment Strategies
One of Oriental medicine’s foundational principles emphasizes that every individual is unique. That is, even if two people present with similar complaints, the cause of illness for one person almost certainly differs from that of the other. Therefore every person’s course of treatment must be individually-tailored to suit his/her particular need. Digestive disorders usually respond best to a combination of three types of therapies: Acupuncture is the insertion of sterile, thin needles into specific sites on the body. Selecting appropriate acupuncture points regulates proper qi or energy flow, which encourages one’s body to bring itself back into balance. When treating digestive disorders, acupuncture can help strengthen the Spleen and Stomach, regulate metabolism, and is especially useful in curbing GI-related acute pain. Chinese Herbal Medicine (CHM) is a science and art supported by at least 2,000 years of empirical practice. Medical practitioners have always prescribed herbs to aid in digestion, promote nutrient absorption, and adjust appetites. Modern research is also finding CHM to be useful in the gastroenterology department. Please see the “research” section below for more on that topic. For example, a study published in 1998 in the Journal of American Medical Association found that CHM individually formulated provided significant, long-term relief for sufferers of irritable bowel syndrome (IBS). Nutrition is an essential component of good general health, and it is an especially important aspect for those with digestive disorders. Understanding a person’s dietary habits and nutritional needs provides the framework for implementing specific, effective dietary changes. The suggested changes usually involve introducing nutritious and delicious foods into the diet rather than depriving one of particular cravings. Often, simple dietary changes make a profound difference within one week.
Western Medicine’s Approach
The Western Medicine treatment of digestive disorders obviously depends on what is being presented. Broadly speaking, Western medicine tends to address the symptoms of a medical condition with medications such as antacids, antibiotics, steroids, laxatives, etc. If symptoms persist, more radical procedures such as surgical intervention may be used.
What Does the Research Say?
A large body of work is building up around the topic of Oriental Medicine and digestive disorders. One of the studies that gained wide recognition early on was a 1998 article that appeared in the Journal of the American Medical Association. In this randomized, double-blind, placebo-controlled trial concerning irritable bowel syndrome (IBS), it was found that both standardized and individually-tailored Chinese herbal formulas significantly improved the bowel symptoms and global quality of life experienced by IBS sufferers in the short term. However, at the 14-week follow-up, only those subjects who took the individually-tailored herbal formulas had sustained improvement(2). An aspect of acupuncture that makes it so versatile is its ability to have a homeostatic effect on the body. For example, whether one has an overactive or underactive digestive system (i.e. diarrhea vs. constipation), acupuncture can help to regulate the disorder, and bring the system back into balance. This effect was studied by Xu, et al. In 2006, who found that the stimulation of acupuncture points traditionally used to treat digestive symptoms accelerated gastric emptying in patients with delayed bowel responses, and relieved dyspepsia in subjects with normal gastric emptying(3). One of the most promising fields for the use of acupuncture is in the field of functional gastric disorders. “Functional disorder” refers to any condition in which the function, or normal operation, of the body is disrupted, but at the same time, exams show no identifiable anatomical or structural abnormalities. In these cases, Western medicine has much difficulty finding the appropriate treatment modalities. Because Oriental medicine views the person as a whole, the treatment approach of a “functional disorder” is no different from other disorders. Clinical research is recognizing that acupuncture may be useful in functional disorders “because it has been shown to alter acid secretion, GI motility, and visceral pain”(4). As such, acupuncture is showing promise in the treatment of gastroesophageal reflux disease (GERD), functional dyspepsia (FD), irritable bowel syndrome (IBS), postoperative nausea/vomiting, and even visceral hypersensitivity(5).
References
1 - Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. National Center for Health Statistics. Vital Health Stat. 1999;10(200). 2 - Bensoussan et al. Treatment of irritable bowel syndrome with Chinese herbal medicine: a randomized controlled trial. JAMA. 1998 Nov 11;280(18):1585-9. 3 - Xu, et al. Electroacupuncture accelerates solid gastric emptying and improves dyspeptic symptoms in patients with functional dyspepsia. Dig Dis Sci. 2006 Dec;51(12):2154-9. 4 - Takahashi, T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol. 2006 May;41(5):408-17. 5 - Ibid

Do the Needles Hurt?
How Safe Is Acupuncture?
Acupuncture is remarkably safe with only 220 adverse events identified in a systematic review of 98 papers reported from 22 countries in 35 years between the time frame from 1965 to 1999. (1)
Do The Needles Hurt?
During the initial visit we discuss your medical history, and perform a physical examination. The physical examination consists of checking your pulse on your wrists, looking at the tongue and performing diagnostic palpations, which involves the pressing of specific reflex zones both on the abdomen and neck region. The palpation will offer further insights into the exact nature of the case. The resulting treatment plan may consist of weekly treatments or treatments every two to three weeks using acupuncture, custom tailored herbal medicine, dietary assessment, and stress reduction techniques.
How Long Do The Visits Last?
The initial visit includes your full health history, examination, an acupuncture treatment, and herbal formulas (if necessary) and can last anywhere from 1 ½ to 2 hours. During the initial visit we also take a close look at your diet and will give you insights how your diet might impact your allergies. We will assist you in making recommendations that help to build your immune system. Follow-up visits usually last about one hour to one hour and 15 minutes. The acupuncture points are chosen carefully at each visit to specifically treat your current individual diagnosis and symptoms. They include points on your arms, legs, back or abdomen. The needles are extremely thin, and typically there is very little discomfort. Most patients enjoy acupuncture and feel deeply relaxed during their treatments. Many patients fall asleep. In addition to needles we may use cupping for your allergic problems. Cupping involves the placement of suction cups usually on your back to help move stagnation and release tension.
How Many Treatments Will I Need?
Since all treatments are custom-tailored this really depends on your specific circumstance. The frequency of treatments will depend on your situation. In severe allergy situations we may want to see you weekly for a couple or three visits then decrease the frequency as you begin to improve. Here at MHS, our practitioners have decades of experience, and are always happy to work with you and your doctor in order to best fit your needs.
References
1. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83.

Complementary Care for Cancer Patients with Chinese Medicine
How can Chinese medicine assist my western cancer therapies?
 As Chinese Medicine (CM) is gaining popularity, more evidence is showing that it can assist cancer patients during their process of conventional treatment. Acupuncture and in some situations, also Chinese herbs, have shown alleviation of many of the common side effects of radiation and chemotherapy. This results in improvement of quality of life for many patients.
As Chinese Medicine (CM) is gaining popularity, more evidence is showing that it can assist cancer patients during their process of conventional treatment. Acupuncture and in some situations, also Chinese herbs, have shown alleviation of many of the common side effects of radiation and chemotherapy. This results in improvement of quality of life for many patients.
What does the research show?
In the past few years, acupuncture and CM have been the focus of increased interest and research funding. The National Institutes of Health (NIH) awarded grants for the first acupuncture trials in 1973. The Society of Acupuncture Research (SAR) promotes research in acupuncture and Chinese medicine, and was actively involved in the November 1997 Consensus Development Conference on Acupuncture, sponsored by the NIH. The panel concluded that, "...there is sufficient evidence of acupuncture's value to expand its use into conventional medicine and to encourage further studies of its physiology and clinical value." (1) The panel found considerable evidence that CM decreases nausea/vomiting during chemotherapy and relieves pain. (2) The American Cancer Society, on its website, states, "Acupuncture is an effective treatment for nausea caused by chemotherapy drugs and surgical anesthesia." (3,4,5) Keith I. Block, MD, Medical/Scientific Director of the Institute for Integrative Cancer Care, states: "Serious exploration of alternative ways to improve the quality of life for persons undergoing cancer therapy represents a cornerstone as we face a new era in the treatment of this insidious disease. This can be accomplished by reducing pain, nausea and other debilitating 'side effects' - and most importantly, to give hope where it has perhaps diminished. As part of an integrative practice, I believe acupuncture has a solid and scientifically promising basis. Thus, continued investigation of acupuncture for clinical application and research is warranted in the area of cancer treatment.” (6) W. Weiger, MD advises patients who seek complementary and alternative therapies for cancer: "Another potential role of acupuncture in patients with cancer is the palliation of chronic pain. Several case reports and series suggest that acupuncture may provide relief when conventional measures fail to control chronic pain resulting from underlying disease or conventional treatments (surgery or radiation). ... In summary, randomized controlled trials to date, suggest that it is certainly reasonable to accept the use of acupuncture in conjunction with standard anti-emetics to control chemotherapy-related nausea and vomiting” (7,8,9,10,11,12,13,14,15) Acupuncture has shown efficacy for advanced breast and lung cancer patients with dyspnea (difficulty breathing) when compared to a sham group. (16) In a University of Pittsburgh Cancer Institute study, researchers received a grant of $1.2 million from the NIH to establish the role acupuncture may play in the treatment of patients with advanced colorectal cancer. "For many terminally ill colorectal cancer patients, their final months are marred by distressing physical and psychological symptoms," remarked Dr. Ellen Redinbaugh, the study's principal investigator. She added that the high hospitalization rates for such patients "indicate a clear need for new interventions to ameliorate their distress and promote their quality of life," and that "acupuncture holds promise as one such technique." (17) How safe is acupuncture? Acupuncture is remarkably safe with only 202 serious adverse events identified in a systematic review of 98 papers reported from 22 countries in 35 years between 1965 to 1999. (18) What is the role of Chinese herbs for cancer patients who are undergoing conventional treatments? Chinese herbs also hold much promise in treating cancer patients. Chinese herbal medicine, just like acupuncture, can be used to relieve nausea in chemotherapy patients. Some patients are intolerant to the side-effects of standard anti-emetic or analgesic drugs, and can benefit significantly from acupuncture and herbal compounds combined. (19) In a study with 182 cancer patients receiving chemotherapy, 98 were also given an herbal formula. It was modified to address issues like poor appetite, leukopenia, hemorrhaging of the digestive or respiratory tract, pain, jaundice, and nausea/vomiting. After 28 days, results observed for the group taking herbs in comparison to the group taking chemotherapy alone were reduced leukopenia and thrombocytopenia, improved appetite and increased body weight. Follow-up after five years revealed that recurrence and metastasis for the chemo/herb group was at 10 percent whereas for the chemo-alone group it was 35 percent. Mortality rates were at 8 percent for the chemo/herb group and 20 percent for the chemo-alone group. (19) Several studies were done to test the effectiveness of radiotherapy when combined with Chinese herbal medicine. White blood and platelet counts tend to stay normal longer in radiation therapy patients with the inclusion of herbs, allowing patients to complete their prescribed courses of conventional treatments with increased potential for success. (20) Primary lung cancer patients were divided into two groups, one group received radiotherapy and CM combined, the other was treated with radiotherapy alone. In the combined group, 69 percent were able to complete their prescribed radiation course, while in the radiation alone group, only 31 percent could complete the course. Tumor circumference showed greater reduction using the combined approach. (20) University of California researchers have found that Chinese herbs used with cancer patients “reduce the tumor load; prevent recurrence or formation of a new primary cancer; bolster the immune system; enhance the regulatory function of the endocrine system; protect the structure and function of internal organs and glands; strengthen the digestive system by improving absorption and metabolism; protect bone marrow and hematopoetic function; and prevent, control, and treat adverse side-effects caused by conventional treatments for cancer.” (22) In the practice of CM, cancer is viewed as a part of a pattern of disharmony both stemming from and affecting the entire system (body-mind-spirit). CM views the imbalanced system as a potential amplifier of cellular aberrations. The main treatment strategy is to restore health by creating homeostasis within the system.
What can I expect?
Patients can expect to receive 5 to 9 treatments over the course of three months in conjunction with ongoing chemotherapy and/or radiation therapy protocols at a cost of approximately $700-$1400. There is very little insurance coverage for acupuncture in North Carolina. Cash, checks and credit cards are accepted. Follow-up treatments can be coordinated with conventional treatment protocol regimens.
How many treatments will I need?
Since all treatments are custom-tailored this really depends on your specific circumstance. Patients have particularly benefited from weekly treatment during the actual chemotherapy and/or radiation to improve their quality of life, but, again, the frequency will depend on your situation. During western medical treatment breaks it can be helpful to build up your immune system, improve digestion and increase your stamina. Here at MHS, our practitioners have decades of experience, and are always happy to work with you and your doctor in order to best fit your needs.
Testimonials:
“I just love getting treatments. They are so relaxing. I hardly notice the needles going in and then, right after the needles go in, I feel this total relaxation coming over me that feels so nourishing, I can hardly describe it. I feel like I am in a trance state. A wonderful feeling!” A. J., Durham, NC “I was originally diagnosed with breast cancer in December of 2003. After surgery, I received the traditional treatment – chemotherapy and radiation. Eleven months after completing that treatment the cancer was back. Remembering the unpleasant side effects of the earlier chemo (low red and white blood counts, lack of energy, nausea and digestive problems), I decided to pursue Oriental medicine as a complementary treatment. This was done with the complete support of my oncologist. We focused the treatment (acupuncture, herbs, diet, etc.) on improving my general health during chemotherapy and countering the negative side effects. We paid special attention to my immune system and were able to keep my white blood counts high enough that I did not get sick or have to skip any chemo treatments. My overall energy and well being have been amazing. I would highly recommend the use of Oriental medicine as a complement to traditional medical treatment.” V. E., March 2006 “I was diagnosed with lung cancer November 2003 and began chemotherapy in February 2003. During treatment, at the urging of my daughter who had greatly benefited from acupuncture, I made an appointment with MHS. The teaching was very powerful for my symptoms, my strengths and weaknesses, my history. The practitioner at MHS was extremely knowledgeable about whole body healing and the importance of the immune system. I truly believe that acupuncture played a key role in my immune system staying strong through 4 months of chemotherapy. I continue to periodically go for acupuncture and I continue to do well as a cancer survivor. Thank You, MHS” J. M. S., April 6, 2006 “When I was diagnosed with my cancer, I was distraught. I was petrified of the upcoming chemotherapy, radiation therapy and surgery. I knew nothing about acupuncture but went to see a practitioner at MHS at the suggestion of a friend. My husband stayed with me after the practitioner put the needles in and says my face relaxed for the first time since the diagnosis and then my body relaxed. He says my spirits improved from that moment forward. After my 4th week of radiation therapy and the 2nd week of in-patient chemotherapy, I was so nauseous that I could keep nothing down. The meds my doctors gave me did little to improve my nausea and I was becoming weaker and battling dehydration. I was hospitalized an extra time just to deal with the nausea and dehydration. By putting needles in my wrists the nausea disappeared immediately. We worked out a way to keep tiny needles in place and I began to regain my strength.” V. P., April 2006 “Six months ago, I was diagnosed with a very early stage breast cancer (ductal carcinoma in situ), for which it was recommended I have a lumpectomy and a six week course of radiation. After the first surgery, I had to have a re-incision, to make the margin around the tissue that was removed and the rest of the breast tissue wider. At the same time, I was bitten by a tick and contracted Rocky Mountain Spotted Fever. After the acute stage of this painful infection abated, I began the radiation treatments on my breast. I truly do not know how I would have made it through both surgeries, the radiation and recovered from the tick-borne disease with out the benefit of acupuncture and other advice from MHS. I had a remarkably rapid recovery from all of these conditions. Thanks to the acupuncture treatments, nutrition advice and a nutritional supplement recommended by a practitioner @ MHS, I experienced less fatigue that many other breast cancer patients. And compared to the other patients I met in the radiation waiting room, I also experienced much milder side effects from the radiation. In fact, my skin never burned, I had no lymph edema and was able to carry on almost normally throughout the six week radiation treatment period. In addition, my recovery from the RMSP was remarkably rapid. I've read and been told by others who had this illness or knew someone who had it, that recovery can take years. I'm pretty much back to my normal functioning and energy levels after six months. Acupuncture and electronic stimulation have also aided in the process of weaning my body off of the powerful narcotic pain medicines that were necessary in the first few months for both recovery from the breast surgery and the RMSF. I am absolutely convinced by my own experiences, that acupuncture and the knowledge of the practitioner helped my body both meet and recover from some very serious challenges much more rapidly than would otherwise have been possible. I am grateful to MHS for the knowledge and assistance that have helped me return to an active and productive life style.” N. S. O'D., April 2006
References:
1. NIH Consensus Panel. Acupuncture. NIH Consensus Development Statement. Bethesda, MD, Nov 3-5, 1997. 2. Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J R Soc Med. 1996. 89.303-311. 3. American Cancer Society. www.cancer.org. 4. Shen J, et al. Electroacupuncture for Control of myeloablative chemotherapy induced Emesis: A randomized controlled trial. JAMA, 2000. 284(21):2755-2761. 5. Beinfeld H, Korngold E. Chinese medicine and cancer care. Altern Ther Health Med. 2003;9(5). 6. Block KI. Acupuncture Complements Cancer Therapy. Acupuncture Today. February, 2003, Vol 04,(02). 7. Weiger W, Smith M, Boon H, et al. Advising patients who seek complementary and alternative therapies for cancer. Annals of Internal Medicine 2002;137:899-903. 8. King CR. Nonpharmacologic management of chemotherapy-induced nausea and vomiting. Oncol Nurs Forum 1997;24 (suppl. 7):41-48. 9. Rhodes VA, McDaniel RW. Measuring nausea, vomiting and retching. In: Frank-Stromberg M, Olsen SJ (eds.) Instruments for Clinic Health Care Res, 2nd ed. Boston, Jones & Bartlett,1997,pp.509-518. 10. de Aloysio D, Penacchioni P. Morning sickness control in early pregnancy by Neiguan point acupressure. Obstetrics and Gynecology 1992;80:852-854. 11. Belluomini J, et al. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study. Obstetrics and Gynecology 1994;84:245-248. 12. Fan CF, et al. Acupressure treatment for prevention of postoperative nausea and vomiting. Anesth Analgesia 1997;84:821-825. 13. Dibble SL, Chapman J, Mack KA, Shih A. Acupressure for nausea: results of a pilot study. Oncology Nursing Forum Feb 2000;27(1):41-7. 14. Pomeranz B. Acupuncture Analgesia-Basic Research, Stux G, Hammershlag R (eds), Clinical Acupuncture: Scientific Basis, Berlin:Springer-Verlag, 2001. pp. 1-29. 15. Alimi D, et al. Analgesic effect of auricular acupuncture for cancer pain: A randomized, blinded controlled trial. J Clin Oncol, 2003. Vol 21(22):4120-4126. 16. Vickers AJ, et al. Acupuncture for dyspnea in advanced cancer: a randomized, placebo-controlled pilot trial. BMC Palliat Care, 2005 Aug 18,4:5. 17. Study examines acupuncture to alleviate symptoms for advanced colorectal cancer patients. EurekAlert news release, March 4, 2003. 18. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83. 19. Wong R, Sagar CM, Sagar SM. Integration of Chinese medicine into supportive cancer care: a modern role for an ancient tradition. Cancer Treatment Reviews 2001;27:235-246. 20. Li Peiwen. Management of Cancer with Chinese Medicine. Donica Publishing, 2003. Distributed by Churchill and Livingstone. pp. 76-77. pp 79. 21. Zhang RJ, et al. Medicinal protection with Chinese herb compound against radiation damage. Aviat Space & Environ Med. 1990;61:729-31. 22. Tagliaferri M. et al. Complementary and alternative medicine in early stage breast cancer. Seminars in Oncology, Vol 28, No 1(Feb), 2001:127.
Book Resources:
Guide to the Causes and Prevention of Breast Cancer. Janette D. Sherman, MD

Breast Pain Associated with Lactation
 Beginning in 2004, the practitioners of Meridian Health Solutions have been working in conjunction with the lactation consultants at UNC-Chapel Hill to study the use of acupuncture in treating breast pain associated with lactation. For the purpose of this study, all patients referred have received western treatment for one month without positive results. Given that the lactation consultants at UNC are among the best in the region, these referrals are generally considered to be the most recalcitrant and difficult-to-treat cases around. We find that our average results at MHS to date (as of December, 2007) are at 1.8 treatments to completely clear this complaint for the nursing duration of the current baby. We have had one patient drop out of the study who had severe multi-systemic complicating factors, for whom we were of no help. Otherwise, everyone has responded positively (n=12). All patients are properly draped during these treatments and no needles are ever inserted into their breasts, making this a safe and comfortable treatment process. Most patients experience an improvement in pain and breast tissue softness between the start and end of a single treatment. We look forward to continuing to affirm acupuncture’s utility for lactation pain with this study over the coming years.
Beginning in 2004, the practitioners of Meridian Health Solutions have been working in conjunction with the lactation consultants at UNC-Chapel Hill to study the use of acupuncture in treating breast pain associated with lactation. For the purpose of this study, all patients referred have received western treatment for one month without positive results. Given that the lactation consultants at UNC are among the best in the region, these referrals are generally considered to be the most recalcitrant and difficult-to-treat cases around. We find that our average results at MHS to date (as of December, 2007) are at 1.8 treatments to completely clear this complaint for the nursing duration of the current baby. We have had one patient drop out of the study who had severe multi-systemic complicating factors, for whom we were of no help. Otherwise, everyone has responded positively (n=12). All patients are properly draped during these treatments and no needles are ever inserted into their breasts, making this a safe and comfortable treatment process. Most patients experience an improvement in pain and breast tissue softness between the start and end of a single treatment. We look forward to continuing to affirm acupuncture’s utility for lactation pain with this study over the coming years.
Traditional East Asian Medicine Treatment Strategies
One of Traditional East Asian medicine’s foundational principles emphasizes that every individual is unique. That is, even if two people present with similar complaints, the cause of illness for one person almost certainly differs from that of the other. Therefore every person’s course of treatment must be individually-tailored to suit his/her particular need. This, of course, applies equally to a woman complaining of plugged ducts during lactation. Acupuncture is the insertion of sterile, thin needles into specific sites on the body. Selecting appropriate acupuncture points regulates proper qi or energy flow, which encourages one’s body to bring itself back into balance. When treating breast pain during lactation, acupuncture can help regulate the energy flow thereby reducing the pain. Pain is usually caused by what Chinese medicine calls “stagnation”, therefore, the treatment is aimed toward opening the energy channels and removing energy stagnation. Sometimes women complain of yeast problems during this phase of their life which can also be helped by Traditional East Asian medicine. Chinese Herbal Medicine (CHM) is a science and art supported by at least 2,000 years of empirical practice. Medical practitioners have prescribed herbs for post-partum complaints for centuries. This form of therapy can be useful for lactating women as well, with unique herbal formulas recommended for specific conditions. Nutrition is an essential component of good general health, and is an especially important aspect for those with plugged ducts associated with lactation. Understanding a young mother’s and her baby’s dietary and nutritional needs provides the framework for implementing specific, effective dietary changes. The suggested changes usually involve introducing nutritious and delicious foods into the diet. Often, simple dietary changes make a profound difference within one week.
Western Medicine’s Approach
Western medicine can offer antibiotic or antifungal medications in cases of bacterial and fungal infections in a lactating woman. These medications can be oral or topical. However, a common conundrum is that when a woman has a bacterial infection, the antibiotics that treat the infection often are the cause for a consequent fungal infection. In the absence of identifiable infection, lactation consultants will work with a nursing mother to identify possible causes of lactation pain, such as vasospasm of the areola, improper breastfeeding positioning, or poor latch-on by the infant. Remedies for these conditions may include warm compresses, dietary supplements, and of course correcting the infant's latch.
What Can I Expect During a Session?
During the initial visit we discuss your medical history, your baby’s nursing history, take a careful look at your dietary habits, and perform a physical examination. The physical examination consists of checking your pulse on your wrists, looking at the tongue and performing diagnostic palpations around the abdomen and neck region. We may ask you to find the most painful area on your breast(s) yourself while we palpate other areas on your body with the intention of releasing the pain in your breasts. The palpations offer further insights into the exact nature of your situation. The resulting treatment plan consists of acupuncture, and we may suggest custom-tailored herbal medicine, nutritional changes, and stress reduction techniques.
Testimonials:
I just had to write and let you know that the treatment worked! After I got home yesterday evening, I pumped milk and immediately noticed a strong stream coming from the right breast that was unusual as of late, and sure enough, the entire breast started emptying and is completely unblocked. Last night, I got the best sleep I'd had since giving birth. Thank you so much for helping me. So far, the breast is continuing to work well. The left breast is also doing well, although I may want to focus on it either Monday or in a later treatment, since it does have one or two small lumps that come and go. Hope you are having a great weekend and will see you Monday morning. Regards, A. B., Chapel Hill, NC My gosh, all this pain I’ve had for all this time. It’s been so tough feeding my little girl. It was gone in only one treatment! I am truly amazed and didn’t think that was possible. THANK YOU! F. W., Durham, NC
References
1. Lao L. et al. Is Acupuncture Safe? A Systematic Review of Case Reports. Altern Ther Health Med 2003;9(1):72-83 2. Medical Errors, http://www.tivcme.com/pme/introduction_index.htm

Allergies and Immunity
What Is The Western View?
 From a Western point of view, allergic rhinitis is caused by an overreaction of the body’s immune system to foreign particulates or allergens including, pollen, dust, molds, dander and environmental toxins. An inflammatory response occurs, releasing histamines and leukotrienes, which cause sneezing, itchy and watery eyes, nasal congestion, headache, runny nose, and possibly sinusitis.
From a Western point of view, allergic rhinitis is caused by an overreaction of the body’s immune system to foreign particulates or allergens including, pollen, dust, molds, dander and environmental toxins. An inflammatory response occurs, releasing histamines and leukotrienes, which cause sneezing, itchy and watery eyes, nasal congestion, headache, runny nose, and possibly sinusitis.
What Is The Western Treatment?
Western Medicine tends to treat allergies in three ways. The first approach involves the use of anti-histamines or anti-leukotrienes, either over the counter (i.e. claritin, benadryl) or by prescription (i.e. Allegra, Singulair). The second type of treatment involves the use of nasal steroids such as nasonex or flonase to reduce swelling and inflammation from the histamine response. Finally, some are treated with injections to the particular allergen to decrease the body’s histamine response.
How Can Traditional East Asian Medicine Help Me?
Traditional East Asian medicine views allergies as a deficiency in the body’s immune system or Defensive qi. A strong Defensive qi prevents the body from responding to allergens in any adverse way. However, when one’s Defensive qi is weak, the body reacts to allergens via an inflammatory response. This response to the allergen is known as “Wind”. Wind could be likened to “air-borne pathogens”. This Wind causes the symptoms of allergies by disrupting the normal energetic functions of the body. The Lungs, which are the immune system’s most vulnerable organ, are especially susceptible to Wind invasions. Traditional East Asian medicine recognizes a distinction between Wind Cold and Wind Heat. Wind Cold manifests with predominant cold symptoms such as clear phlegm, sneezing, body aches, watery eyes; Wind Heat exhibits predominantly heat symptoms such as green or yellow phlegm, itchy, red eyes, and possibly associated fever.
What Does Traditional East Asian Medical Treatment Entail?
A randomized controlled study looked at true vs. sham acupuncture and concluded that active acupuncture was more effective than sham acupuncture in decreasing the symptom scores for persistent allergic rhinitis and increasing the symptom-free days. No serious adverse effect was identified. (1) Acupuncture and Chinese herbal medicine have been shown to be effective in treating allergies by stimulating and strengthening the body’s immune system, regulating the immune response and alleviating the signs and symptoms of allergic rhinitis. A randomized controlled study looked at 52 patients with chronic seasonal allergic rhinitis. The control received acupuncture to non-acupuncture or sham points and a non-specific herbal decoction. The study group received a semi-standardized treatment of acupuncture and a prescribed Chinese herbal decoction. The results showed an 85% improvement in the study group and only a 40% improvement in the control group. The study group also showed a significant improvement after treatment on the VAS (visual analogue scale) and the rhinitis quality of life questionnaire. (2) Treatments are designed to each individual’s needs depending on what signs and symptoms are present. Studies show that treatments are more effective when patients take herbs specifically for their needs in addition to acupuncture. This also cuts down the overall cost of treatment, as the patient gets daily support between the acupuncture treatments, thus requiring fewer acupuncture treatments.
How Does Traditional East Asian Medicine View The Immune System?
The body’s immune system or Defensive qi regulates the complex interactions between normal cells and possible pathogens such as viruses, bacteria, micro-organisms and other toxins to prevent or fight infections. The body depends on proper sleep, nutritious diet, and exercise to maintain this defense system. Other factors such as over exposure to harmful pathogens, excessive use of antibiotics, and stress can weaken a healthy immune system. Once depleted, we become more susceptible to colds, flus, and allergies. At the same time, it is more difficult to overcome these ailments. Acupuncture and Chinese herbal medicine have been used for thousands of years to improve and support the immune system. In addition, it can support the body by eliminating the pathogens and can reduce and/or resolve the symptoms from such infections.
References:
1. Daniel K. Ng, FRCP, et al. A Double-Blind, Randomized, Placebo-Controlled Trial of Acupuncture for the Treatment of Childhood Persistent Allergic Rhinitis. Pediatrics. Vol. 114 No. 5 November 2004, pp. 1242-1247 2. Brinkhaus, B., et al. Acupuncture and Chinese herbal Medicine in the treatment of patients with seasonal allergic rhinitis: a randomized-controlled clinical trial. Allergy, 2004; 59 (9), 953-960.